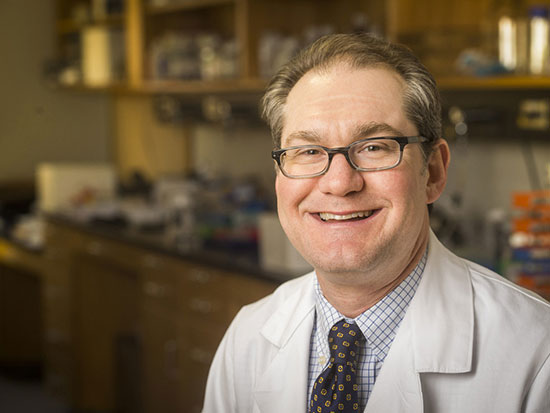
 "How do you specifically test for COVID antibodies? We're working on that," said Randall Davis, M.D., recipient of one of 14 pilot grants to accelerate urgent COVID-19 research at UAB.What's the secret to a strong antibody response against COVID-19?
"How do you specifically test for COVID antibodies? We're working on that," said Randall Davis, M.D., recipient of one of 14 pilot grants to accelerate urgent COVID-19 research at UAB.What's the secret to a strong antibody response against COVID-19?
Plans affecting billions of people worldwide are resting on the answer to that question. Priming antibodies to attack is the idea behind vaccines, of course. And in the months or years before a successful vaccine arrives, many governments have pinned their hopes of reopening on widespread antibody testing to identify people who have already been exposed to SARS-CoV-2, the novel coronavirus that causes COVID-19. But that is a lot of weight to bear for tests that rest on a series of scientific unknowns.
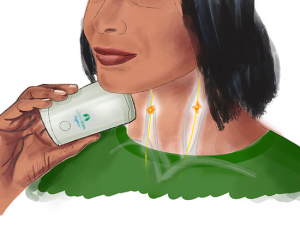
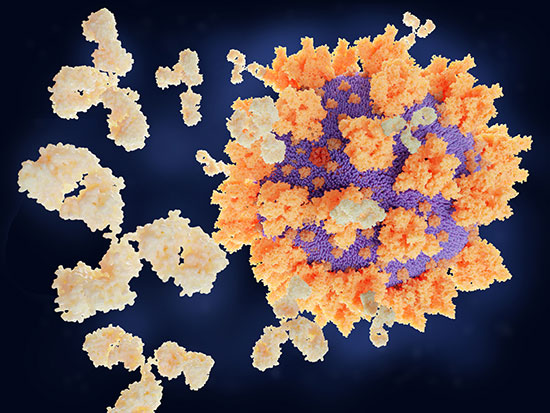
The tests themselves are straightforward: they look for antibodies in a patient's blood that can bind to pieces of the virus that the human immune system is most likely to recognize — primarily the prominent spike proteins that stud the outside of SARS-CoV-2.
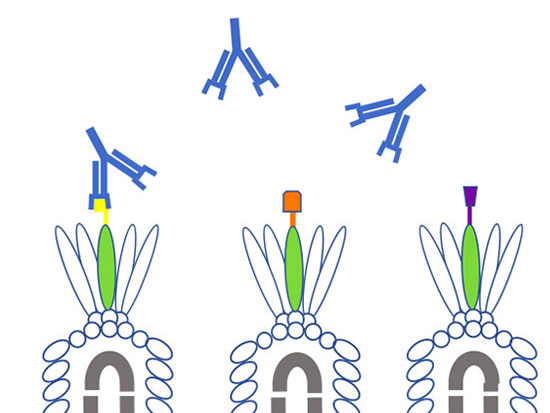
Antibodies are not created equal, however; some are stronger than others. Strong, in this sense, means they bind tightly to key spots on SARS-CoV-2 and provide host protection. Clinicians and researchers are especially interested in antibodies that interfere with the virus’s receptor binding domain — the area on the tip of the spike protein that interacts directly with the ACE2 receptors on the human cells SARS-CoV-2 is trying to invade. These so-called neutralizing antibodies are exactly the type that clinicians want for convalescent plasma therapy — in which antibodies from recovered COVID-19 patients are transfused into patients fighting the disease. (Learn more in this related story.) But current antibody tests aren’t designed to evaluate antibodies with this specificity.
| "We're looking for really good antibodies that can block viral entry into human cells. That will help us identify potential candidates who could donate their plasma to people who really need them.” |
Finding the best anti-COVID antibodies, and figuring out exactly how they interact with SARS-CoV-2, is the focus of a new UAB pilot project — one of 14 internal projects selected for the School of Medicine's $1.1 million Urgent COVID-19 Clinical Research and Laboratory Research Fund.
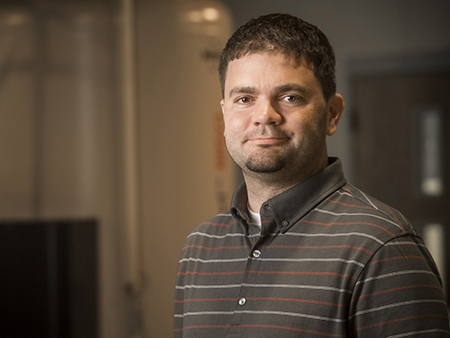
"We're looking for really good antibodies that can block viral entry into human cells,” said Randall Davis, M.D., principal investigator on the project, professor in the Department of Medicine in the School of Medicine and a senior scientist in the O'Neal Comprehensive Cancer Center at UAB. “That will help us identify potential candidates who could donate their plasma to people who really need them.”
Davis has already seen the power of these convalescent plasma treatments (so-called because antibodies reside in blood plasma, the liquid part of the blood). "I have a patient with leukemia and she contracted the SARS-CoV-2 virus," Davis said. "She was admitted to the hospital, got somewhat better and went home. She did poorly for three weeks, got readmitted to the hospital and wasn't doing well. Another family member had the virus and cleared it. The blood types matched, so the family member donated their plasma and designated it for my patient. Now they have recovered and gone home. That's why I got involved in this."
Related story:

Convalescent plasma therapy is treating coronavirus patients in UAB research
How can you tell quality antibodies from weaker specimens? Start by embedding key parts of SARS-CoV-2, such as its receptor binding domain, on a fixed plate. "Then you pass the serum at different titrations over the spike protein and we see if ACE2 can bind it," Davis said. "You may not see blockade at any dilution; that means that person didn't generate the right immune response. If they did, you can find at what concentration or dilution it disappears. If you are making truckloads of this antibody, and it blocks the spike protein from binding to ACE2, you're probably a good candidate to donate plasma."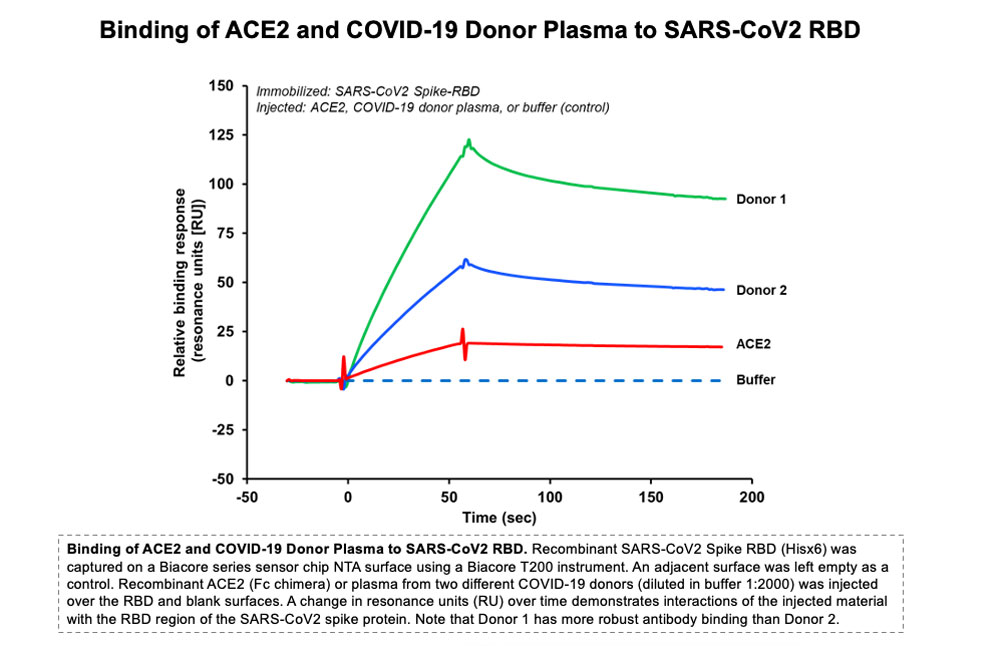
Davis's lab is equipped with a specialized surface plasmon resonance instrument "that allows you to determine very sensitive binding between macromolecules in real time," he said. (Davis runs the Multidisciplinary Molecular Interaction Core facility at UAB.) This instrument, known as a Biacore, “is used for drug screening, antibody screening — any time you are trying to figure out the binding between one or more things," Davis said.
 Detailed information on antibody binding properties in SARS-CoV-2 can help overcome other limitations in current antibody tests, Davis said. One is the possibility of "cross-reactivity" — false positive results that occur when tests mistakenly flag antibodies to another coronavirus. In addition to SARS-CoV-2 and the original SARS virus, there are several other coronaviruses that affect humans, including two responsible for a good chunk of common colds, Davis said. (The RNA sequence to make nucleocapsid proteins for SARS-CoV-2 is around 90% identical to the sequence for the original SARS, for instance.) "Any kid who has been to daycare has likely had a coronavirus," he said. "Many people have generated antibodies against some type of coronavirus." These antibodies clearly could spark a false positive result on a SARS-CoV-2 antibody test, but exactly how common is this? "That's a big gap in our understanding: How do you specifically test for COVID antibodies?" Davis said. "We're working on that."
Detailed information on antibody binding properties in SARS-CoV-2 can help overcome other limitations in current antibody tests, Davis said. One is the possibility of "cross-reactivity" — false positive results that occur when tests mistakenly flag antibodies to another coronavirus. In addition to SARS-CoV-2 and the original SARS virus, there are several other coronaviruses that affect humans, including two responsible for a good chunk of common colds, Davis said. (The RNA sequence to make nucleocapsid proteins for SARS-CoV-2 is around 90% identical to the sequence for the original SARS, for instance.) "Any kid who has been to daycare has likely had a coronavirus," he said. "Many people have generated antibodies against some type of coronavirus." These antibodies clearly could spark a false positive result on a SARS-CoV-2 antibody test, but exactly how common is this? "That's a big gap in our understanding: How do you specifically test for COVID antibodies?" Davis said. "We're working on that."
| “I don't think I've ever appreciated living in Birmingham more than now. We have an outstanding medical center and staff. The quality of the types of faculty here and the resources that we have are really outstanding." |
Another part of Davis's project will focus on the evolution of the immune response against SARS-CoV-2, which draws in many different subtypes of cells and antibodies as it fights off infection. "We're looking at the kinetics of those antibodies," Davis said. "The virus has different structural parts to it. What parts of the virus are the antibodies recognizing? And in particular, is a person making antibodies that can block the spike protein and its receptor binding domain? If you want to make a system to prevent the virus from entering you would want to make antibodies against this spike protein." This information will be useful to groups developing vaccines and treatments to fight COVID-19.
He is hardly the only person working on the problem, Davis pointed out. "There are probably 100s of labs doing this same type of thing on the planet," he said. Still, he said that UAB has unique resources that position it to be a leader in this area. "In a lot of ways, UAB has been blessed," Davis said. "The collaborative environment we have; the Center for AIDS Research here, which has had an international reputation for many years; infectious diseases experts such as Paul Goepfert, Mike Saag, Sonya Heath and Jeanne Marrazzo. I don't think I've ever appreciated living in Birmingham more than now. We have an outstanding medical center and staff. The quality of the types of faculty here and the resources that we have are really outstanding."
Read more on UAB's urgent COVID-19 research projects

Glow-in-the-dark coronavirus testing is first project of new hire

Researchers model COVID-19 infection in 3D human lung tissue

Tackling his third pandemic, UAB researcher gets up close with coronaviruses in order to kill them

Researchers are creating a coronavirus showdown to settle pressing antibody problems
Helpful viruses may unlock the secrets of coronavirus antibodies
Cytokine storm treatment for coronavirus patients is focus of first-in-US study
UAB launches research studies to combat COVID-19