
Curriculum Overview
In the UAB Pediatric Residency Program, our curriculum is aimed at providing a superb foundation in general pediatrics. We offer an ABP eligible pathway and a non-ABP eligible pathway. This foundation fully prepares residents for future careers both in outpatient general pediatrics and for subspecialty training. Our graduates and those who employ them consistently report that our program has fully prepared them for fellowship or for independent practice. Over the last 10 years, about half of UAB Pediatric graduates have entered general pediatrics settings, while the other half have gone on to academic subspecialty fellowships.
UAB graduates are leaders in their fields. Department chairs, residency program directors, division directors, biomedical researchers, NIH Study Section Chairs, journal editors, a past president of the American Academy of Pediatrics, and countless community pediatric leaders got their start in the UAB residency program.
Sample Block Schedules
-
PGY-1
Block 1
Pediatric Hospital Medicine
Block 2
Pediatric Hospital Medicine
Block 3
Subspecialty Rotation
(GI/Pulm/
HemOnc
/Renal)Block 4
Subspecialty Rotation
(GI/Pulm/
HemOnc
/Renal)Block 5
Newborn Hospital Medicine
Block 6
Ambulatory Immersion
(Primary Care, subpecialty clinics)Block 7
Night Float
Block 8
Night Float
Block 9
NICU
Block 10
General Pediatrics Foundations
Developmental & Behavioral Pediatrics
(1 week)
Community Pediatrics (1 week)
Mental Health Education (1 Week)
IPCA (1 Week)Block 11
Pediatric Emergency Medicine
Block 12
Elective
Continuity Clinics
Average two full days per month on inpatient rotations
Vacation
Three weeks total taken during Elective, Ambulatory Immersion and PEM months. One week vacation per year during Thanksgiving, Christmas or New Years. One unscheduled week at the end of the year.
For more information about nights and call click below for a PDF of the sample block schedule.
-
PGY-2
Block 1
Pediatric Hospital Medicine
Block 2
Subspecialty Clinic
Block 3
Subspecialty Individualized
CurriculumBlock 4
Subspecialty Individualized
CurriculumBlock 5
Developmental & Behavioral
Pediatrics
(3 weeks)
Mental Health
(1 week)Block 6
Elective
Block 7
Night Float
Block 8
NICU
Block 9
PICU
Block 10
PICU
Block 11
Pediatric Emergency Medicine
Block 12
Pediatric Emergency Medicine
Continuity Clinics
Average two full days per month on inpatient rotations
Vacation
Three weeks total taken during Elective, Ambulatory Immersion and PEM months. One week vacation per year during Thanksgiving, Christmas or New Years.
For more information about nights and call click below for a PDF of the sample block schedule.
-
PGY-3
Block 1
Pediatric Hospital Medicine
Block 2
Pediatric Hospital Medicine
Block 3
Subspecialty Individualized
CurriculumBlock 4
Subspecialty Individualized
CurriculumBlock 5
Adolescent
Block 6
Health Department
Block 7
Night Float
Block 8
Career Intensive Month
Block 9
Elective
Block 10
Elective
Block 11
Subspecialty
Block 12
Pediatric Emergency Medicine
Continuity Clinics
Average two full days per month on inpatient rotations
Vacation
Three weeks total taken during Elective, Ambulatory Immersion and PEM months. One week vacation per year during Thanksgiving, Christmas or New Years.
For more information about nights and call click below for a PDF of the sample block schedule.
Rotation Overview
-
Inpatient Pediatrics at Children’s of Alabama (General & Subspecialty)
Inpatient teams are resident-led teams, even when rounding with a fellow. Residents lead family-centered rounds and develop and implement plans for patient care. Attending physicians are present each day on rounds for supervision, guidance, and education. On inpatient services with fellows, fellows assist in the supervision and teaching of residents and students.
-
Pediatric Hospital Medicine (PHM)
Pediatric Hospital Medicine (PHM) teams provide care for about 1/3 of the inpatient admissions at Children's of Alabama. Because Children's of Alabama is both the local children's hospital for the greater Birmingham area and the referral center for all of Alabama and parts of neighboring states, the PHM service cares for a diverse patient population with a wide range of diagnoses.
-
Attendings are members of the Division of Pediatric Hospital Medicine and are leaders in education, quality improvement, and advocacy at UAB and nationally.
-
Each PHM team consists of an attending, three pediatric residents and one to three medical students.
-
Each team is also assigned a social worker, case manager, and pharmacist to assist with follow-up appointments, patient teaching, working with DHR, coordinating prescriptions, along with many other services.
-
Each team has a cap of 15 patients (intern cap of eight patients), with a max of eight patients admitted on a call day.
-
Patients are admitted to PHM teams using a “drip system” until 3 p.m. during the week and 12 p.m. on holidays and weekends. After this time, the call team (short call every fourth day) admits all patients until 5p.m. This allows each team to get new patients daily. Overflow patients are admitted by a separate attending hospitalist team.
-
A separate night float team is in house at 5 p.m. to perform cross-cover and admissions.
-
Ward teams participate in monthly simulation cases to enhance their learning.
-
Our complex care service (“Teal Team”) is staffed by 1-2 residents, nurse practitioners, and our complex care attendings. Junior residents will cross-cover these patients while on night float with assistance from their senior residents.
-
-
Newborn Hospital Medicine
Residents in their first year of training spend one month caring for infants in the Mother-Baby Unit of UAB's Women and Infants Center. Goals of this rotation include developing skills in the evaluation and care of healthy newborns. Residents gain expertise in newborn physical exam and circumcision skills and learn about a variety of topics including neonatal jaundice, sepsis, feeding difficulty, breastfeeding, evaluation of heart murmurs, and anticipatory guidance.
-
Neonatal Intensive Care
A total of two months during residency is spent in the 120 bed, level III+ Regional Neonatal Intensive Care Unit (RNICU), also located at UAB’s Women and Infants Center. As one of the largest and busiest NICU’s in the nation, residents can expect to see a wide range of patients ranging from extremely low birth weight premature infants to critically ill full-term neonates. Residents attend all high risk or otherwise complicated deliveries and thus become proficient at resuscitating newborns on this rotation. Additionally, residents have the opportunity to perform numerous procedures including intubations, umbilical line placement, and lumbar punctures. Residents are also exposed to the management and care of neonates with cardiac lesions while in the NICU.
While in the NICU, interns work on a night float system with an average of five to seven overnight shifts during the rotation and the remainder of shifts occurring during the day. Upper level residents work on a hybrid scheduling system with night float coverage Monday through Thursday.
-
Pediatric Intensive Care
Second-year pediatric residents spend two months in the Pediatric Intensive Care Unit (PICU) at Children’s of Alabama. This 24-bed unit provides state-of-the-art, critical care for the sickest children in the state and region. Residents gain in-depth experience in the identification and management of respiratory and cardiac failure, treatment of sepsis, management of severe trauma, post-operative complications, and a wide range of other disorders. This experience provides confidence to manage sick patients for the remainder of our residents' careers. Residents also hone their procedural skills with intubations, line placement, and other diagnostic procedures during these rotations.
While in the PICU, care is supervised by pediatric critical care trained faculty and fellows. Residents work on a night float system with one week of nights during their month and the remaining shifts occurring during the daytime.
-
Pediatric Emergency Medicine
Like most urban children’s hospitals, the Children’s of Alabama emergency department (ED) cares for a wide array of problems ranging from routine pediatric concerns to acute, life-threatening trauma, and illnesses. With an average 70,000 annual patient visits and 400 traumas (of which >25% are Level I) managed in 54 single patient rooms and four state-of-the-art trauma bays, the Children’s of Alabama ED allows our residents significant hands-on experience managing every level of acuity. During the Pediatric Emergency Medicine rotation, residents provide initial contact and care with supervision from fellowship-trained Pediatric Emergency Medicine specialists. Resident shifts range from 8-10 hours and vary between daytime, afternoon/evening, and an average five to seven overnight shifts throughout each month of service.
-
Pediatric Subspecialty Rotations
The UAB Pediatric Residency Program offers subspecialty exposure to the full array of pediatric experiences. Subspecialty rotations include allergy/immunology, cardiology, endocrinology, gastroenterology, genetics, hematology-oncology, infectious disease, nephrology, neurology, pulmonology, rheumatology. In each subspecialty, residents have the opportunity to work with fellowship trained faculty, many of whom are renowned in their respective field. Subspecialty rotations are spread throughout the three years of training and include a mix of inpatient service, consult, and outpatient care experiences for residents.
-
Outpatient Pediatrics
Residents spend an average of one ½ day per week in our continuity clinic at the Pediatric Primary Care Clinic (PCC). The PCC is located in the Park Place building directly adjacent to the hospital. Residents serve as the general pediatricians for children from the surrounding community and are each assigned a patient panel of approximately 100 patients, ranging from newborns to 18-year-olds with a variety of medical conditions and complexities. Residents also enjoy working with the same PCC pediatrician as their attending throughout the three years of residency to establish further continuity and mentorship.
As part of the outpatient pediatric education, residents also rotate through various outpatient clinics including Adolescent Medicine, Sparks Center at UAB, subspecialty clinics at Children’s of Alabama, Jefferson County Health Department community care clinics, and a number of community private pediatric offices. Residents also practice taking after-hours calls for the resident PCC during two weeks of their second year.
-
Adolescent Medicine
All residents complete a one month experience in adolescent medicine. This rotation provides the basis for evaluation and care of this special pediatric population. Training locations include the inpatient and outpatient facilities of the Children’s of Alabama as well as focused instruction in eating disorders clinic, juvenile detention centers, weight management clinics, adolescent HIV clinics, adolescent gynecology clinics, and a teen transition clinic.
-
Developmental and Behavioral Pediatrics
An understanding of typical and atypical behavior and development are key foundations of training in pediatrics, as such every resident experiences one month of developmental and behavioral pediatrics (DBP). Working alongside fellowship trained DBP-faculty, residents will enjoy experiences in DBP Clinic, Autism Clinic, Trisomy 21 Clinic, Muscular Dystrophy Clinic, Newborn Follow-up Clinic for former premature infants, Spina Bifida Clinic and sessions with occupational and physical therapy.
-
Electives
Individualized curriculum is important for career development. In addition to rotating on services relevant to desired career paths, residents also receive four electives during which they can craft their own learning experiences ranging from inpatient or consult services to outpatient, general to subspecialty exposure, personal development or research, and everything in between. Program directors and chief residents support residents in developing electives in line with their goals. Use the Elective Catalog link below to view some of the historically popular elective rotation experiences.
Scholars Programs
The UAB Pediatric Residency Program offers five scholars programs to provide residents the opportunity to gain expereince in the target areas of medical education, health disparities, global health and rural health. Click on the program title below to learn more about each program.
-
Pediatric Residents Interested in Medical Education (PRIME) Scholars
Pediatric Residents Interested in Medical Education (PRIME) Scholars is a longitudinal learning experience designed to provide pediatric residents with skills and knowledge to become excellent medical educators. Components of the program include: 1) monthly group discussions, 2) observation and evaluation of resident teaching, and 3) scholarly projects.
Pediatrics PGY-2 and PGY-3 residents and Med-Peds PGY-2 through PGY-4 residents are eligible for the program. The application and selection process takes place in the Spring.
Current Participants
PGY-2: Anna Dickson, Deena Elsheikh, Sarah Hicks, Dalton Hall, John Charles Nichols, Emily Hooker, Jessica Costero, Tabitha Kearns.
PGY-3: Ryan Boykin, Matthew Harberg, Meredith Goldenberg, Sam McCartney, Maggie McCartney, Lauren Oliver, Daniel Cooper, Owen Chandler, Jessica Corners.
PGY-4: Giavanna Verdi.
Chief Residents: Anna Seidenburg & Megan Weber - Med-Peds
Goals
PRIME Scholars will become proficient clinical teachers in a variety of settings, including at the bedside, in small groups, and large group settings. Scholars will gain skills to effectively lead clinical teams in a manner that promotes learning, including establishing expectations and providing individual feedback. They will gain an appreciation for processes through which high-quality medical education scholarship is conducted. Through implementation of teaching strategies gained in the PRIME Scholars program, participants will enhance the education of UAB medical trainees, including medical students and co-residents, as well as fellows and faculty.
Scholarly Projects in Progress or Development Stage
-
Chalk Talk Templates to Promote Teaching on Pediatric-Hospital Medicine and Hematology/Oncology Rotations
-
Improving Handoff Through Use of I-PASS
-
Noon Conference Workshop to Improve Peer-Peer Feedback
-
Exploring Strategies to Increase Morning Report Attendance
-
PGY-1 Procedure Day/Transition to Upper-Level Talk
-
Peer Mentor Program
Faculty Leaders
Will Sasser, M.D.
Associate Professor, Division of Pediatric Critical Care
Associate Program Director, Pediatric Residency ProgramMichele Nichols, M.D.
Professor, Division of Pediatric Emergency Medicine
Program Director, Pediatric Residency ProgramBrian May, M.D.
Assistant Professor, Division of Pediatric Hospital Medicine
Assistant Program Director, Combined Medicine-Pediatrics Residency ProgramChristina Cochran, M.D.
Associate Professor, Division of Pediatric Emergency Medicine
Assistant Program Director, Pediatric Emergency Medicine Fellowship ProgramAnnalise Sorrentino, M.D.
Professor, Division of Pediatric Emergency Medicine
Career Development Director, Pediatric Emergency MedicineCarlie Stein, M.D.
Assistant Professor, Division of General Internal Medicine
Program Director, Combined Medicine-Pediatrics Residency ProgramErinn Schmit, M.D. M.Ed.
Assistant Professor, Division of Pediatric Hospital Medicine
Assistant Program Director, Pediatric Hospital Medicine Fellowship ProgramAndrew Watson, M.D.
Assistant Professor, Division of Pediatric Hospital Medicine -
-
Health Equity Scholars Program
The Health Equity Scholars Program aims to equip pediatric and combined pediatric residents, as well as pediatric subspecialty fellows, with the skills to lead improvements in child health equity. This is achieved through a comprehensive learning experience that includes both instructional sessions and hands-on community engagement.
PGY-1: Barbara Awad, Gisseth Mora Scarpetta, Bella Blair.
PGY-2: Amelia Hartje, Deena Elsheikh, Erin Carriker, Virginia Quinlan, Jessica Robinson.
PGY-3: Carson Huynh, Jessica Corners, Harshadayani Jagadish Kumar, Stephanie Smith.
PGY-4: Renita Daniels
Goals
By the conclusion of the Health Equity Scholars Program, participants will:
-
Become pediatricians with outstanding clinical skills who also understand the full range of determinants of health and barriers to health care.
-
Develop a foundational knowledge of resources available to overcome barriers in health care to promote exceptional care is provided to vulnerable and populations from disadvantaged backgrounds
-
Develop leadership, communication, scholarship and advocacy skills to advance health equity.
-
Learn to design, implement, and evaluate interventions through quality improvement initiatives to improve child health equity.
-
Develop a framework for educating others on barriers to health equity for vulnerable and populations from disadvantaged backgrounds
Curriculum Overview
-
Monthly didactic and experiential learning sessions
-
Group QI Project
-
Two weekend long immersive experiences in regions of Alabama per year (Fall and Spring)
Faculty Leaders
Lece Webb, M.D.
Assistant Professor, Division of Pediatric Critical Care
Director of Fellowship Programs Access & Engagement InitiativesNicole Jones, M.D.
Assistant Professor, Division of Pediatric Emergency MedicineChrystal Rutledge, M.D.
Associate Professor, Division of Pediatric Critical Care
Madura Hallman, M.D.
Assistant Professor, Division of Pediatric Critical Care -
-
Pediatric Underserved and Global Health (PUGH) Scholars Program
The Pediatric Underserved and Global Health (PUGH) Scholars Program is a unique opportunity for pediatric residents to gain experience and focused education in global health during the 3 years of residency training. We are looking for residents with a passion for practicing medicine in underserved communities to reduce healthcare disparities and a desire to experience global health both here in the U.S. and abroad. Residents will gain an understanding of the general principles related to health in developing countries and providing culturally sensitive and competent care in a limited resource setting.
The program will give priority to Pediatrics and MedPeds PGY-1 residents but is open to upper level residents if there are spots available. The application and selection process takes place in the Spring. Three residents will be selected for the program each application cycle.
PGY-1: Lauryn Bass, Alyssa Goldman, Kahlea Haladwala, Jacob Wurst
PGY-2: Kymberlee Evans, Rafaella Navarro Hoyos, Jemma Thompson
PGY-3: Maya Ahmadieh, Shaun Kuo, Elizabeth Proenza, Joshua Self
Goals
-
To provide structured education for pediatric residents surrounding global health principles
-
To prepare residents to address healthcare delivery and work to eliminate healthcare disparities in the global underserved population
-
To provide mentorship for a career in global heath as well as pre-departure planning and scholarship oversigh
-
To recruit strong resident applicants interested in global health
-
To foster longitudinal partnerships with global sites for bidirectional mentorship, education, and research
Curriculum
-
Attend at least 2/3 of the global health meetings
-
Quarterly Global Health Noon Conference
-
Quarterly Global Health Morning Report
-
Global Health Interest Group Meetings
-
-
Spend your non-call elective during 3rd year in an underserved setting (either here in the U.S. or overseas)
-
Target overseas sites: Kijabe, Kenya; Santiago, Chile (2021-2022 academic year); Lusaka, Zambia
-
US sites: Indian Health Services; Black Belt, Alabama; Health Department; other rural Alabama location
-
Other sites may be acceptable on case by case basis
-
-
Complete a scholarly project (anything from a reflective essay to an advocacy, QI, or research project)
Faculty Leaders
Meghan Hofto, M.D.
Assistant Professor, Division of Pediatric Hospital MedicinePriya Prabhakaran, M.D.
Professor, Division of Pediatric Critical Care
-
-
McDonald Scholars Program
The McDonald Scholars Program provides the opportunity for interested residents to enhance their general pediatric learning with a two week immersion experience in a rural or underserved community. Residents selected as McDonald Scholars will be paired with an established pediatric practice for a two week clinical experience as a way to further learn and truly encompass what being a pediatrician in a rural or underserved area entails.
The program is open to rising PGY-2 and PGY-3 Pediatric or PGY-2 through PGY-4 Med-Peds residents and accepts applications in the spring. Four to eight residents will be selected each year to participate in the program.
PGY-2: Amelia Hartje, Suzannah Patterson, Maddie Southall, Michael Padgett, Jemma Thompson and Danielle Windom.Goals
-
To give residents an “immersion” type experience in a rural practice in Alabama
-
To provide and engage our residents in a different underserved population
-
To strengthen the General Pediatric experience of our residents
-
To inspire and possibly peak interest in a rural type practice
-
To honor the generous giving of Dr. and Mrs. Jack McDonald.
Faculty Leaders
Michele Nichols, M.D.
Professor, Division of Pediatric Emergency Medicine
Program Director, Pediatric Residency ProgramCandice Dye, M.D.
Associate Professor, Division of Academic General Pediatric
Associate Program Director, Pediatric Residency Program -
-
Primary Care Scholars Program
The Primary Care Scholars Program was launched in 2024 in order to increase primary care exposure for residents through three separate arms: clinical exposure, mentoring, and focused didactic education. All residents interested in learning more about primary care careers are welcome to attend the didactic and networking activities below, even if they have not formally joined the Scholars Program.
The clinical experience portion of the scholars program is open to PGY-2 and PGY-3 Pediatric or PGY-2 through PGY-4 Med-Peds residents and accepts applications in the Spring. Two residents are selected each year to receive funding for the clinical experience.
Clinical Experiences
Residents selected to participate in the scholars program are paired with a community pediatrician for a 1 month elective during their PGY-2/3 year where they will have the opportunity to shadow and provide direct patient care to pediatric patients in the ambulatory setting.
In the PGY-3/4 year they will have the opportunity to participate in a transition to independent pediatric practice (TIPP) elective where they will have the opportunity to build skills that will benefit them in serving as a practicing pediatrician in the community.
Didactic Education
Throughout the year, all residents interested in primary care are invited to attend monthly didactic teaching sessions on primary care specific topics during the lunch hour.
Topics to be covered include: nutrition counseling, behavioral challenges in pediatric patients, pediatric mental health topics, academic underachievement and navigating school accommodations, breastfeeding, motivational interviewing, transition to adult care, complex care management.
Mentoring/Networking
Quarterly All scholars and residents interested in primary care are invited to attend General Pediatric Society aka “GPS” socials which are hosted by general pediatric faculty at their homes in the evening to allow residents and community pediatricians an opportunity to meet outside of the clinical setting and facilitate networking and mentorship for residents interested in careers in primary care.
2025-2026 Scholars
PGY-2: Maddie Southall
PGY-3: Daniel Cooper
Goals
-
To give residents exposure to high volume community general pediatric clinical practice.
-
To increase resident mentorship with community pediatrician faculty.
-
To strengthen the General Pediatric didactic educational opportunities for our residents
Faculty Leaders
Channing Brown, M.D.
Assistant Professor, Division of Academic General Pediatrics
Assistant Program Director, Internal Medicine-Pediatrics Residency ProgramCaroline Densmore, M.D.
Assistant Professor, Division of Academic General Pediatrics -
Simulation Education
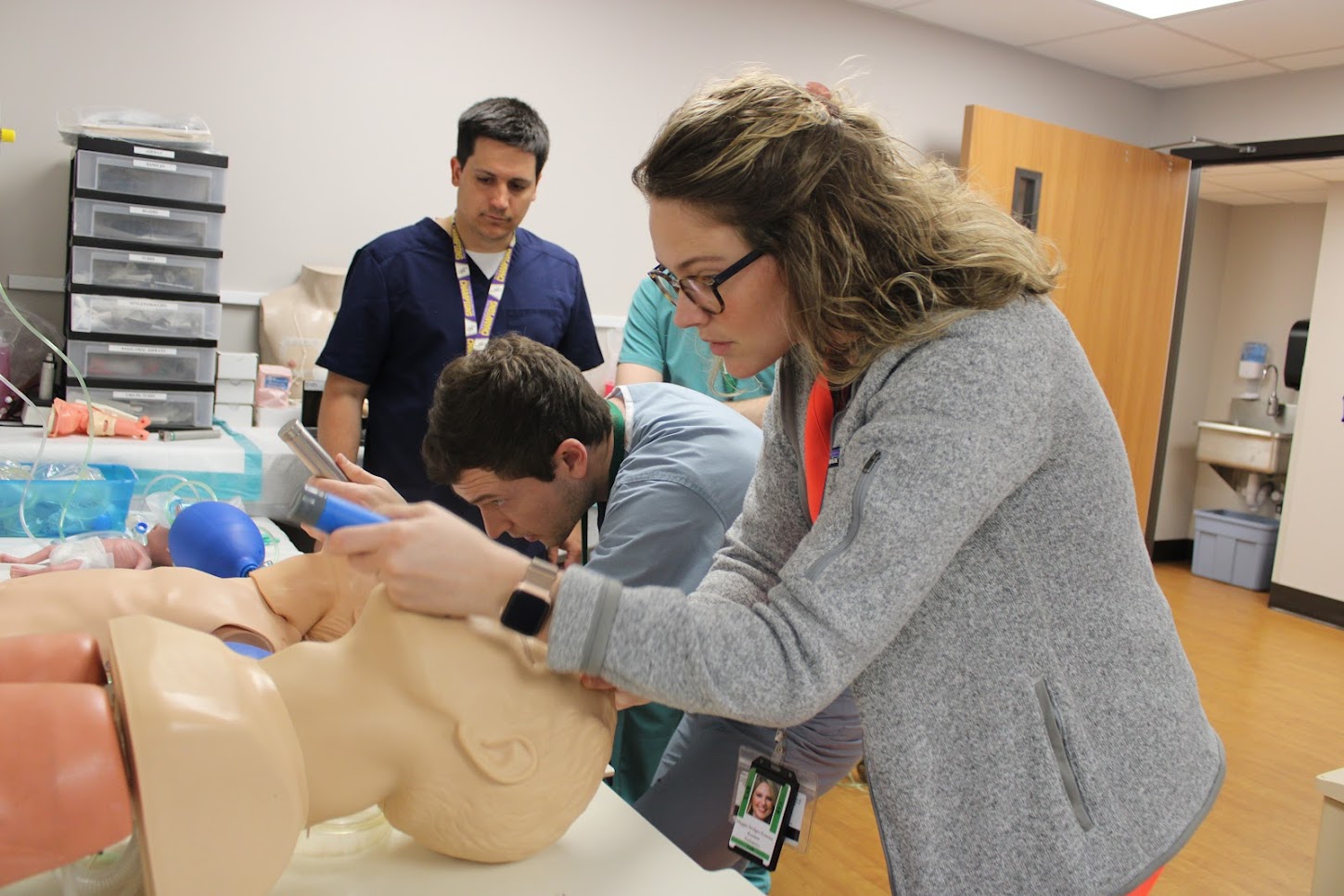
Interns are introduced to the Simulation Center during orientation with simulated check-out of patients, care of ill children, and procedures including: lumbar punctures, I/O placement, intubations, umbilical line placement, etc. Simulation continues throughout residency during most inpatient months. For example, residents in the PICU (during 2nd year) attend a weekly Critical Care Simulation. Mock codes (using the Simulation Center simulators) are also performed on a monthly basis in various locations around the hospital.
The Children's of Alabama Simulation Center is always growing. Currently, it has 12 patient simulators ranging from premature newborn to teenager. The Simulation Center is the only pediatric simulation center in the state of Alabama. In May 2025, the simulation center welcomed it's 100,000th learner.
For more information on the Simulation Center click here.
Daily Education
-
Stagno Morning Report

On June 18, 2014, the UAB Pediatrics Residency Program renamed Morning Report to Stagno Report in honor of Dr. Sergio Stagno for his dedication to the residency program and the education of residents. The Stagno Report takes place every morning at 7:55 in the Bradley Lecture Center. Cases are generally presented by upper level residents and led by the chief residents. Residents on PHM, subspecialty rotations, PICU, NICU, and emergency medicine present on a rotating basis, discussing a wide variety of cases. In addition we have longitudinal general outpatient pediatrics, social determinants of health, ethics, and global health discussions as well. The Stagno Report is always well attended by residents, medical students, fellows, and attendings alike. It is interactive with resident and attending participation concerning the history, physical exam, differential diagnosis, and management of the day’s case presentation. Because of these aspects, an engaging discussion takes place every morning, with multiple learning points.
-
Journal Club
Journal Club occurs on a monthly basis in the morning during Stagno Report. Residents are provided an article as well as relevant questions ahead of each meeting to facilitate engaging conversation. Articles are chosen by our residents and cover a wide variety of topics relevant to pediatric residency training.
-
Noon Conference
Noon conference takes place every Monday, Tuesday, and Wednesday in the Bradley Lecture Center. Residents are provided with a free, hot meal on a daily basis during these lectures. In addition, all residents’ pagers are held and answered by the chief residents so that the residents will be able to spend the hour focused on the lecture. Noon conferences are given by faculty and staff. The material covered includes an expansive review of pediatric medicine topics relevant to both clinical practice and board preparation.
In July of each year, there is a special series presented that covers basic patient care and emergency situations among the Pediatric subspecialties, to provide a foundation of knowledge for residents and interns.
Senior Talks are given once per month, and take place during the noon conference hour. Two of the senior residents (third-year categorical pediatrics and fourth-year med-peds residents) present a 30 minute evidence-based medicine talk on a topic of their choice.
Every Thursday, residents are offered opportunities during their noon hour to attend Pediatrics Grand Rounds or interest group meetings to further advance their education and explore their career goals.
Board Preparation
For the past 10 years (2014-2023), we have had a 98% Board pass rate.
In addition to exposure to a wide breadth and depth of patients and excellent teaching by our attendings and fellows, we also have several programs in place in our curriculum to help prepare for the Pediatric Boards:
-
Board Review Series
Board Review Series
Starting in January, we have weekly lectures hosted by attending and fellows from every department to review pearls and tips for the Boards. After the lecture, the presentations and recorded lectures are made available to residents for review as needed.
-
American Academy of Pediatrics PREP®
American Academy of Pediatrics PREP®
The UAB Pediatric Residency Department pays for every resident's annual AAP membership throughout residency. This provides residents with access to at least three years of board content-based “PREP questions." Residents are required to complete one year’s worth of these questions during each year of training (approximately 250 questions per year).
-
Pediatrics in Review®
Pediatrics in Review®
As part of the residents’ funded AAP memberships, the Pediatrics and Pediatrics in Review journals are both delivered on a monthly basis to all of our residents, which is a great source of review for basic pediatrics topics.
-
Question of the Day
Question of the Day
Every morning, before Stagno report, residents answer a Board-style question. Each month, the intern or resident with the most correct answers is awarded a "Golden Pen".