Mary Duncan, R.N., MSN, CIC, is the senior director of Infection Prevention for the UAB Health System, with 18 years of experience implementing best practices at various health facilities. Her position at UAB places her in charge of preventing infections among patients and staff at one of the largest public hospitals in the country.
Mary Duncan, R.N., MSN, CIC, is the senior director of Infection Prevention for the UAB Health System, with 18 years of experience implementing best practices at various health facilities. Her position at UAB places her in charge of preventing infections among patients and staff at one of the largest public hospitals in the country.
Infection prevention, broadly defined, is any “action that a person can take to prevent a pathogen from entering the body and causing disease,” Duncan said. The good news is that these actions are “something that anyone can learn,” she added.
One of the major lessons of the COVID-19 pandemic is that everyone needs to learn about basic infection prevention measures before it is a matter of life or death, Duncan says. When the pandemic began, “I saw how confused my family and friends were and how quickly they lost faith in the people that they thought they could trust: the government, the CDC, the World Health Organization and even their doctors,” Duncan said. “When people are in the middle of a crisis, they are not really open to learning new things. They fall back on what they know or what they think they know, and it is very difficult to try to trust a new person when you are just trying to survive.”
This article is based on a presentation that Duncan delivered as part of a series organized by UAB’s Alabama Regional Center for Infection Prevention and Control Training and Technical Assistance, or ARC IPC. Watch Duncan’s presentation in full here, and learn more about ARC IPC at sites.uab.edu/arcipc.
Unfortunately, COVID-19 is not likely to be the last serious outbreak we encounter. Of the deadliest disease outbreaks stretching back a century, more than half have occurred in the past two decades alone, Duncan explains. And increasing development worldwide and interactions between humans and animals mean that it is a matter of when, not if, we all have to deal with another disease epidemic, she said: “We have to do a better job of empowering people on how to protect themselves from new pathogens.”
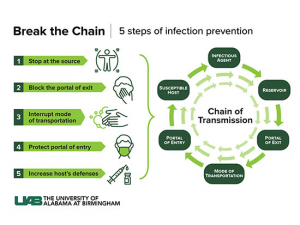
Understanding the chain of transmission
The best place to start, Duncan says, is with a model known as the chain of transmission.
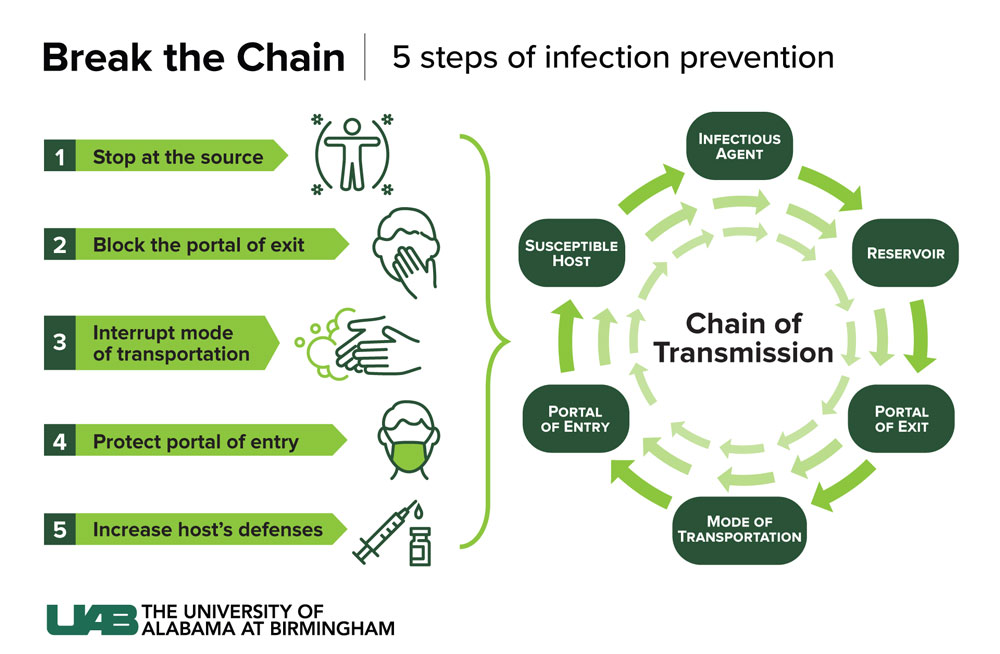
1) Infections start, naturally enough, with an infectious agent. “The most important part of the whole chain of transmission is a pathogen’s being able to enter a susceptible host,” Duncan said. “This means that the pathogen is able to live and multiply in the new host.” For some infectious agents, this can mean colonization, “where the pathogen lives in the tissues but isn’t causing disease,” Duncan said. But as we all know, SARS-CoV-2, the virus that causes COVID-19, is very good at infecting humans.
2) The infectious agent normally lives, grows and multiplies in a reservoir. This might be the environment, an insect or on a surface. Or, as with COVID-19, “the reservoir is mainly humans, although we know it can also live in animals,” Duncan said.
Infection prevention, broadly defined, is any “action that a person can take to prevent a pathogen from entering the body and causing disease,” Duncan said. The good news is that these actions are “something that anyone can learn,” she added.
3) To infect someone new, infections need a portal of exit from their reservoir. For COVID-19 that is the respiratory tract.
4) COVID-19’s mode of transmission is illustrated when a person coughs, sneezes, talks or sings. “The mode of transmission is mainly through direct contact with those droplets, or to some extent some aerosolized particles,” Duncan said. “Research has found that the ability to be transmitted through surfaces is a little less common with COVID-19.”
5) Infecting another person requires a portal of entry, which for COVID-19 is “the eyes, nose and mouth of the new host,” Duncan said.
6) Even once the infectious agent makes it inside another person, that person must be a susceptible host. Again, unfortunately, “the susceptible host with COVID-19 is really any person of any age, although older adults and those with preexisting medical conditions are more vulnerable to becoming severely ill,” Duncan said.
Breaking the chain
To prevent the transmission of a pathogen, infection prevention experts follow a tried-and-true playbook.
1) Stop it at the source
- Eliminate the infectious agent or source. “This can be done by giving an antimicrobial to a patient who has an active infection or treating a wound infection so that no bacteria can go out into the environment,” Duncan said.
- Quarantine exposed individuals during the incubation period. That way, “if the person is to develop an infection, there is no place for them to spread it to,” Duncan said.
- Isolate symptomatic persons. “So there is no new host that the infectious agent can infect,” she said.
- Eliminate the reservoir. Use an approved disinfectant to clean surfaces or the pieces of equipment that the pathogen may be living on.
- Testing and surveillance. This is especially important “to identify where the reservoirs are if a disease has asymptomatic spreaders, like COVID-19,” Duncan said.
2) Interrupt the portal of exit
“If we haven’t been able to kill the reservoir, then we need to move to the next link in the chain and interrupt the portal of exit,” Duncan said.
- Respiratory hygiene/cough etiquette. “Make sure that, if somebody is coughing or sneezing, they are doing it into their elbow or a tissue,” Duncan said. Masks prevent droplets from being dispersed into the environment, “and we found with COVID-19 that masking the source person is very effective in reducing transmission,” she said.
- Clean and cover. Keeping wounds clean and covered is another important method of stopping the spread of infections that are passed on in body fluids or feces.
3) Interrupt the mode of transmission
“If we haven’t been successful yet, then we need to interrupt the mode of transmission,” Duncan said.
- Standard precautions. Hand hygiene, use of gloves, safe injection practices, sterilizing instruments and cleaning environmental surfaces “are an essential practice to prevent the spread of disease,” Duncan said.
- Transmission-based precautions. These are used for highly infectious agents such as flu and the SARS-CoV-2 virus that causes COVID-19. “Anybody who enters the room is required to wear a mask to prevent the droplets from the patient hitting mouths or noses, and then if they are close enough, within 3 to 6 feet, they wear eye protection as well,” Duncan said.
- Adequate ventilation. Over the past several years, “we have learned how important it is to ensure that pathogens are not spread by the air — they are being removed by effective filters or there is enough fresh air coming in to dilute the virus,” Duncan said.
4) Protect the portal of entry
“If the pathogen does find a mode of transmission, there are several things we can do to block entry into our bodies,” Duncan said.
- Masks and eye protection protect the most common access routes.
- Clean and cover. “If we have breaks in our skin, we can make sure they are clean and covered with a bandage,” Duncan said.
- Remove extraneous equipment. In a health care setting, “we can remove any catheters, IVs, drains or tubes when possible so we don’t give pathogens a direct route into our bodies,” Duncan said.
5) Increase the host’s defenses
“And then if all the efforts to break the chain fail and the pathogen makes it into the new host, then there are several things we can do to stop the pathogen from causing an infection,” Duncan said.
- Vaccines. “The number one way to protect people from a potential pathogen is through the administration of an effective vaccine,” she said. “Vaccines have essentially eliminated childhood illnesses that killed or maimed so many children in the past. I’m really one of the first generations who doesn’t know anybody who has had measles, mumps or polio. And my children’s generation is one of the first ones that won’t know anybody who has had chickenpox.”
- Antibiotics. The discovery of antibiotics has revolutionized the fight against pathogens, Duncan said, “but we have learned pretty quickly that we need to be careful with antibiotics, because the pathogens are smart and they can learn how to evade them, so antibiotic stewardship is hugely important.”
- Good health habits. “An individual’s health is so important in protecting them from pathogens,” Duncan said. “Studies have shown that people who smoke or have uncontrolled diabetes or are obese have worse outcomes if they are infected with COVID-19.”
- Personal hygiene. “Removing pathogens from our hands and skin with soap is so important, and then making sure that we have good oral hygiene as well,” Duncan said. “Both of these will prevent reservoirs on our body for the pathogens to live.”