During the fall 2023 semester, UAB students, faculty and staff will have the opportunity to provide feedback and influence UAB’s next strategic plan — Forging Ahead — which will guide continued, purposeful growth for 2024-2028.
During the fall 2023 semester, UAB students, faculty and staff will have the opportunity to provide feedback and influence UAB’s next strategic plan — Forging Ahead — which will guide continued, purposeful growth for 2024-2028.
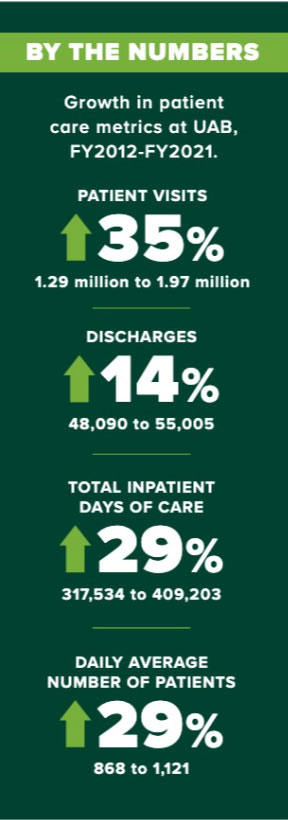
As we look ahead, we revisit the success achieved together through Forging the Future, UAB’s current strategic plan. Here, we celebrate our shared results and positive momentum in the Patient Care pillar of our mission and the 2018-2023 strategic plan.
Patient Care objectives outlined in Forging the Future were to improve patient access and satisfaction through integration of clinical services across UAB’s health care delivery entities, invest in signature treatments that will be delivered through recognized flagship programs, develop infrastructure to ensure statewide access to telehealth services, and integrate engagement throughout the university.
During the life of Forging the Future, the university and Health System significantly increased engagements and collaborations across the enterprise to enhance patient access and care. From student and employee health to training of health care professionals, to combined efforts to battle the COVID-19 pandemic and more, UAB broke down silos and built new and innovative solutions with the institution’s collective brain power and resources.
Patient satisfaction
Patient satisfaction is one of the most important parts of how UAB measures the quality of care and patients’ perceptions of their overall experience.
In 2016, UAB Medicine became the first health care provider in Alabama to make patients’ feedback about their UAB physicians available online as part of its dedication to transparency and accountability.
At the time of launch, more than 81 percent of eligible physicians (those with at least 30 patient-submitted surveys) had a rating of four or five stars on the five-star scale. In 2018, UAB Hospital was one of only three in Alabama to be recognized with an Outstanding Patient Experience Award from Healthgrades.
One major element of the plan developed by UAB Medicine’s Office of Patient Experience and Engagement is to celebrate providers who score the highest ratings across several domains, including “listened carefully,” “demonstrated care and concern,” and “included patient in health care decisions.”
Between 2020 and 2022 alone, more than 270,000 patients used UAB’s real-time patient listening platform to provide feedback about their clinic visits, with “friendly” being the most commonly used word to describe the experience.
In November 2022, UAB Medicine celebrated the 366 highest-scoring providers as part of its fourth annual Ambulatory Provider Recognition Event. Those providers score an average of 95 percent or higher in care satisfaction based on patient feedback — a testament to their service, sacrifice and commitment to patients.
Patient access
 UAB continues to innovate to extend the reach of its expertise and resources to help improve Alabamians’ access to quality health care, launching partnerships through affiliate and management agreements, health authorities, and a strategic alliance that have drastically improved Alabama’s health care ecosystem.
UAB continues to innovate to extend the reach of its expertise and resources to help improve Alabamians’ access to quality health care, launching partnerships through affiliate and management agreements, health authorities, and a strategic alliance that have drastically improved Alabama’s health care ecosystem.
In 2022, Northwest Regional Health, a hospital in Winfield, Alabama, entered into a management agreement to become a member of the UAB Health System, the latest of 13 hospitals across the state to partner with UAB through affiliation or management agreements since 2013.
“With rural hospitals closing across the nation and many threatened in Alabama, we made it a priority to help rural hospitals survive,” said UAB Medicine CEO Reid Jones. “We can leverage our knowledge to create efficiencies and processes that keep hospitals open and — most important — improve the health of patients across the state.”
In April 2020, Jefferson County and the UAB Health System created the Cooper Green Mercy Health Services Authority to provide high-quality health care to all residents of Jefferson County, regardless of their ability to pay. Under the agreement, Cooper Green Mercy Health Services Authority became an affiliate of the UAB Health System, maintaining its status as a full-service ambulatory care facility that has primary and specialty-care clinics, urgent care, physical, occupational and speech therapy, laboratory services, imaging, and pharmacy.
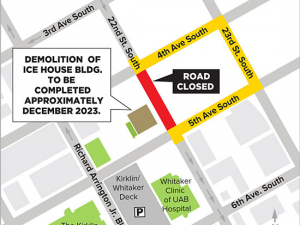
The existing Cooper Green facility, originally called Mercy Hospital when it opened in 1972, will be replaced with a state-of-the-art medical clinic, built on the site of the former Cooper Green parking deck. The new five-story building will be 207,000 square feet, including plans for a magnetic resonance imaging machine, a separate phlebotomy and injection clinic to streamline lab visits and improve the process of vaccinations, and clinic areas designed to support team-based, multidisciplinary care. Construction began in early 2023.
UAB has also expanded patient access by broadening availability of new treatments and studies. Among many examples, UAB was awarded a federal grant of up to $5 million to test whether improving access to telehealth services and access to adequate transportation for those living in rural areas can maintain or improve care quality and lower health care costs; another $3.6 million study is evaluating innovative approaches to help adults with Type 2 diabetes.
 UAB is also helping address a critical lack of access to dental health in Alabama. The American Dental Association ranks Alabama last in the country for access to dental care; 71 percent of the state’s counties are experiencing a dental care shortage. In September 2022, the School of Dentistry announced plans to bring a new satellite dentistry clinic to Dothan to recruit, educate, train and retain dentists. The clinic, supported by a $3.4 million state appropriation, will be able to conduct more than 10,000 patient visits annually and will be staffed by School of Dentistry faculty, residents and dental students.
UAB is also helping address a critical lack of access to dental health in Alabama. The American Dental Association ranks Alabama last in the country for access to dental care; 71 percent of the state’s counties are experiencing a dental care shortage. In September 2022, the School of Dentistry announced plans to bring a new satellite dentistry clinic to Dothan to recruit, educate, train and retain dentists. The clinic, supported by a $3.4 million state appropriation, will be able to conduct more than 10,000 patient visits annually and will be staffed by School of Dentistry faculty, residents and dental students.
Across the country, UAB has set the standard on how to translate advances in dental care and research into everyday practice. In 2012, a seven-year, $66.8-million grant from the National Institute of Dental and Craniofacial Research—at the time, the largest grant in UAB history —established the National Dental Practice-Based Research Network. The network links clinical researchers at UAB and other institutions to practicing dentists.
“These partnerships allow working dental offices to participate in the evaluation of existing and novel strategies for improving oral health for their patients,” said Gregg Gilbert, DDS, director of the National Network and professor and chair of the School of Dentistry’s Department of Clinical and Community Sciences.
The UAB School of Optometry also made strides under Forging the Future to enhance patient care and access to treatment. In 2022, UAB Eye Care launched a new Pediatric Aphakia Clinic – started by Natalie West, OD – in response to increasing demand.
Aphakia is the lack of natural focusing lenses in the eye due to bilateral congenital cataracts. After a child undergoes cataract surgery, surgeons needed help with contact lenses for their pediatric patients. West explains that, unlike most adults who undergo cataract surgery, most infants do not receive implants to replace the natural lens of the eye. The continual changes in eye growth over the first 12-18 months of life and the potential need for more surgeries make implants impossible.
“This leaves the infant with a very high prescription that needs to be corrected in order to provide good visual input to the brain,” she said. “Contact lenses are a great option compared to glasses for some of these patients. Contact lenses offer better visual optics for patients compared to glasses, due to the thickness in the glasses prescription needed for these patients. Contact lenses also allow a better chance of continual wear of the prescription because babies cannot take them out, compared to the babies’ ability to pull at and remove glasses from their face.”
West’s goal is to train future optometrists to continue to increase access to quality eye care for this specialized patient population. Already, many patients and families are driving several hours for this life-changing care at UAB.
Infrastructure for telehealth
Developing infrastructure to ensure statewide access to telehealth services was a key patient care objective in Forging the Future.
In 2016, UAB nephrologist Eric Wallace, M.D., became the first physician in the United States to replace a comprehensive face-to-face visit for a home dialysis patient with a telehealth visit. The visit, part of a pilot study partnership between the Heersink School of Medicine and the Alabama Department of Public Health, allowed Ellen McGowen, 63, to be seen at her local Colbert County Health Department instead of making the 230-mile roundtrip visit to Birmingham.
But there was a long way to go before more Alabamians could benefit similarly. In 2017, Wallace became the system’s first medical director for Telehealth. One challenge was the lack of health insurance parity laws in Alabama (reimbursing providers for telehealth visits at the same rate as in-person visits). Lack of reliable internet access in rural areas, especially for lower-income patients — precisely the population who would most benefit from telehealth — was another obstacle.
Nevertheless, the telehealth team was able to establish partnerships focused on stroke and critical partnerships statewide, and Wallace had developed a workflow for delivering telehealth.
Then came COVID. Suddenly, everyone needed telehealth services, and “over the past two and a half years, we’ve seen how valuable and effective telemedicine has become,” Wallace said. As UAB Hospital prepared for its first wave of COVID cases in March 2020, it was imperative to limit in-person, nonessential visits. By the next month, 74 percent of all ambulatory (outpatient) visits at UAB were using telehealth, and Wallace’s team had trained 2,200 UAB providers in how to use these unfamiliar tools and workflows.
Between March 2020 and March 2022, UAB providers completed more than a half-million telehealth visits. Telemedicine improved the safety and efficiency of treatment for patients with COVID in all health care settings, but particularly in rural hospitals.
 Slow or nonexistent internet access remains a significant obstacle to leveraging the strengths of telehealth to help all Alabamians. In summer 2020, Alabama Governor Kay Ivey appointed Wallace and Curt Carver Jr., Ph.D., vice president for Information Technology and chief information officer at UAB, to serve on the Broadband Working Group, providing input and guidance on investing up to $300 million in CARES Act funding to the state for technology and infrastructure expenditures.
Slow or nonexistent internet access remains a significant obstacle to leveraging the strengths of telehealth to help all Alabamians. In summer 2020, Alabama Governor Kay Ivey appointed Wallace and Curt Carver Jr., Ph.D., vice president for Information Technology and chief information officer at UAB, to serve on the Broadband Working Group, providing input and guidance on investing up to $300 million in CARES Act funding to the state for technology and infrastructure expenditures.
UAB providers continue to prioritize and innovate in telehealth.
Signature programs
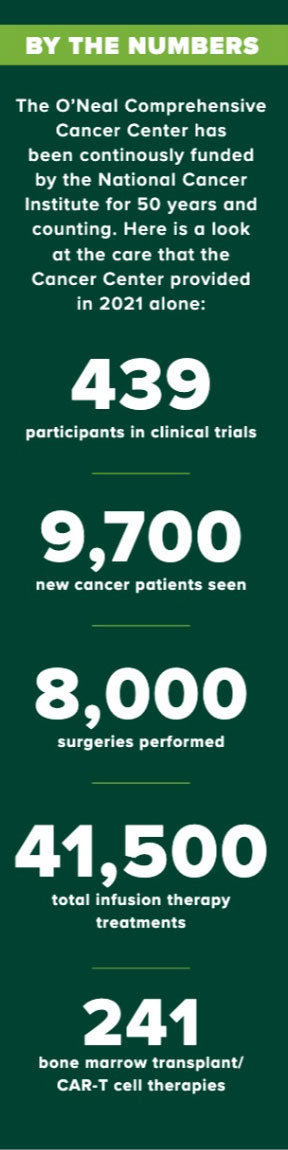
How UAB focused on signature patient care programs during the life of Forging the Future is evident in how we are shaping the future of cancer care.
From its foundation as one of the original eight National Cancer Institute-designated comprehensive cancer centers in 1971 (and still the only one in Alabama and in a four-state region), the O’Neal Comprehensive Cancer Center at UAB has been able to offer patients access to cutting-edge treatments that are available at only a small number of locations nationwide. In June 2022, the National Cancer Institute renewed the OCCC’s Cancer Center Core Support Grant for five years and $27.4 million.
Today, “many patients on clinical trials are experiencing remarkable, disease-altering effects on cancers that were uniformly lethal just yesterday,” said Barry Sleckman, M.D., Ph.D., director of the O’Neal Comprehensive Cancer Center. “For this reason, offering cancer patients clinical trial opportunities is really the standard of care for cancer.”
Despite this, only 3 percent to 5 percent of adult cancer patients in the United States participate in trials, according to a 2019 paper in the journal Oncology. One of the motivations for the $30 million gift from O’Neal Industries, Inc., to name the O’Neal Comprehensive Cancer Center in 2018 was to expand research efforts that could bring additional clinical trials opportunities to UAB and Alabama.
Many of these clinical trials are for new forms of immunotherapy, which has radically changed the treatment outcomes for many patients with cancer. One form of immunotherapy, CAR-T therapy, for example, trains immune cells called T cells how to fight cancer. This form of treatment can be helpful for patients with various cancer types even when other types of treatments are no longer available — so much so that CAR-T therapy has joined surgery, chemotherapy and radiation as one of the pillars of cancer care.
Importantly, starting cancer care has never been easier at UAB, which has streamlined the process with the introduction of the cancer service line, designed to improve the access and coordination of clinical cancer care. It begins with a single phone number for patients, providers and referring physicians to call where they can speak with a live person, instead of an automated system, whose responsibility is to route them to the correct specialists.
“The cancer service line is the glue that holds together cancer care across the entire system,” said Jordan DeMoss, vice president of Clinical Operations for UAB Medicine. “Every cancer patient needs to have the same approach to accessing our system, regardless of what type of cancer they have. It’s care without walls.”
This enables the focus to be specifically on the cancer treatment itself, and not on the various departments and divisions that provide clinical care. Through the cancer service line, obtaining medical records, setting up appointments and testing, and communicating information to the patient are done in a more convenient and timely manner.
See growth recaps of the Research, Community Engagement and Education pillars and learn more about Forging the Future successes in Patient Care and across all UAB mission pillars in UAB Magazine.