By Jennifer Lollar
Using our telehealth expertise, the University of Alabama at Birmingham School of Nursing is working with a local addiction recovery facility to continue to provide primary care during the novel coronavirus (COVID-19) pandemic for underserved patients, helping improve their quality of life and at the same time giving some undergraduate students opportunities for spring clinical hours.
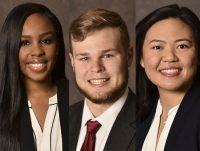
Since January, School of Nursing faculty, including Deborah Bowers, DNP, CRNP, FNP-BC, Michael Mosley, CRNP, ANP-BC, and Emily Patton, CRNP, FNP-C, have had a faculty practice with The Foundry’s Changed Lives Mobile Clinic, serving men at The Foundry’s two residential facilities in Birmingham and Cullman in central Alabama. The clinic is part of The Foundry Rescue Mission and Recovery Center, a faith-based drug and alcohol rehabilitation program.
The faculty, in partnership with the School’s Offices of Technology and Innovation and Clinical and Global Partnerships, have taken the Foundry’s on-site clinic and remade it as a telehealth clinic to continue to provide much-needed care during this time of social distancing.
Maria Shirey, PhD, MBA, RN, NEA-BC, ANEF, FACHE, FNAP, FAAN, Associate Dean for Clinical and Global Partnerships, said it is important the School’s faculty practices continue caring for the underserved during this pandemic.
 “We have a uniquely qualified cadre of nurse practitioners capable of making a distinct difference in the lives of individuals who otherwise would have difficulty accessing primary care,” she said. “Tapping into our School’s telehealth technology makes these opportunities possible.”
“We have a uniquely qualified cadre of nurse practitioners capable of making a distinct difference in the lives of individuals who otherwise would have difficulty accessing primary care,” she said. “Tapping into our School’s telehealth technology makes these opportunities possible.”
Housed in the School’s in-house TeleCare Unit, the clinic is staffed at the School by Bowers, Mosley, Patton and undergraduate students who are working to complete their spring psychiatric mental health clinical hours. One of the clinic’s collaborating physicians — Erin DeLaney, MD, or Jill Marsh, MD, both from the UAB School of Medicine — joins the group virtually, as does the student’s clinical faculty Gary Milligan, DNP, MHSA, RN, CNE. The Unit is set up with spaces between stations to make social distancing optimal.
On site at CLCC and The Foundry Farm are volunteers Amanda Darby Lee, BSN, RN, and Kristina Adkins, BSN, RN, both graduates of the School’s Registered Nurse Primary Care initiative, and pharmacist Kristi Crump, PharmD, RPh.
Lee, Adkins and Crump wear full personal protective equipment, donated by the School’s skills and simulation labs. Lee and Adkins, maintaining social distancing, set up each exam station on site, including a blood pressure cuff, thermometer and oxygen monitor in each room before patients arrive. All items are sanitized before patients arrive and between each patient.
The School’s team worked together to develop a protocol to ensure optimal safety for patients, Lee, Adkins and Crump:
- Participants register beforehand to see the School-based nurse practitioners virtually in 20-minute time slots to promote social distancing.
- They wash their hands before going into one of three stations that connect virtually with a nurse practitioner.
- Participants take their own blood pressure, temperature and oxygen saturation with easy to use devices with the NP supervising/recording.
- After an assessment by one of the School-based nurse practitioners, verbal orders are given to Lee on site if something additional is needed, including blood glucose checks or injections, and new prescriptions or refills also are dictated at this time.
- Lee then cleans exam stations between participants using hospital grade cleaner.
Crump staffs the dispensary at CLCC and The Foundry Farm where patients get new medications or prescription refills, including blood pressure medications and prescriptions for depression or anxiety. She is able to maintain social distancing while ensuring each patient leaves with the medications and other supplies they need.
 “Many of the patients we saw in our first virtual clinic had ongoing health issues that left untreated could potentially be life threatening,” Bowers said. “Many of the men in the program have chronic diseases, high blood pressure or diabetes, and many more have mental health issues that are now compounded by the uncertainty surrounding COVID-19. Maintaining this clinic in the way we have hopefully helps keep CLCC and The Foundry Farm residents in their treatment program and keeps them from going to a local emergency room for primary care.”
“Many of the patients we saw in our first virtual clinic had ongoing health issues that left untreated could potentially be life threatening,” Bowers said. “Many of the men in the program have chronic diseases, high blood pressure or diabetes, and many more have mental health issues that are now compounded by the uncertainty surrounding COVID-19. Maintaining this clinic in the way we have hopefully helps keep CLCC and The Foundry Farm residents in their treatment program and keeps them from going to a local emergency room for primary care.”
“It is important to keep the mobile clinic functional at CLCC and at the Foundry Farm because both ministry campuses serve some of society’s most vulnerable persons,” said CLCC Chief Program Officer Brandon Lackey. “In the midst of an opioid public crisis and a global pandemic, having professionals from the UAB SON available, even from a distance, provides a great deal of comfort to those we serve.”
Professor and Associate Dean for Technology and Innovation Jacqueline Moss, PhD, RN, FAAN, said that while there were a few issues with a slower internet connect on The Foundry’s end, her team, including Clinical Simulation Specialist Sherrie Hafley, who is leading the telehealth implementation for all of the School’s clinics, has worked with The Foundry and the School’s team to solve the issue.
“We pay attention to all the hardware, software and technical requirements to deliver care, so our clinicians don’t have to,” Moss said. “Our goal is the make the experience seamless for clinicians, students and patients at both ends of the internet.”
In the second night of the clinic, where there were no technical issues and all went incredibly well, the undergraduate students joined the faculty and were able to observe NP's as they met patient needs through the telehealth session. Milligan, who observed the group’s first telehealth clinic, created educational materials around the student experience for knowledge and enrichment purposes.
 “Undergraduate students will learn to assess patients through the telehealth option and in summer term be able to utilize therapeutic communication to provide patient education sessions, stress management techniques and medication management,” Milligan said.
“Undergraduate students will learn to assess patients through the telehealth option and in summer term be able to utilize therapeutic communication to provide patient education sessions, stress management techniques and medication management,” Milligan said.
Associate Professor and Associate Dean for Undergraduate and Prelicensure Education Gwen Childs, PhD, RN, FAAN, said this opportunity for undergraduate students is excellent exposure for their psychiatric mental health clinical but also to both population health and telehealth experiences.
“Because the pandemic has affected in-person clinical experiences with patients for pre-licensure students, not just at UAB but across the country, this virtual opportunity not only provides clinical education for program requirements for the undergraduate students, it also is an opportunity at the prelicensure level to learn about current and future technologies for seeing patients and learning about population health and caring for vulnerable populations,” Childs said.
The School’s Registered Nurse Primary Care (RNPC) initiative, supported by a $2.8 million HRSA grant and of which Lee and Adkins are recent graduates, helps to improve health outcomes in medically underserved areas in Alabama by focusing on training and sustaining baccalaureate-prepared RNs and builds on the UAB School of Nursing’s expertise in interprofessional collaborative practice and education for community-based chronic disease management of individuals with complex medical conditions.
Shirey, the RNPC project director said, “It is so rewarding to see graduates of this program such as Ms. Lee and Ms. Adkins making an impactful primary care contribution so soon after graduation.”
Additional sources of funds for equipping the telehealth suite also were provided by the RNPC HRSA grant.