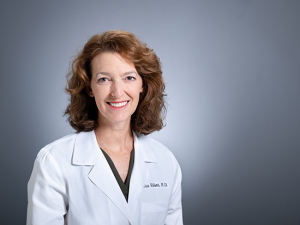
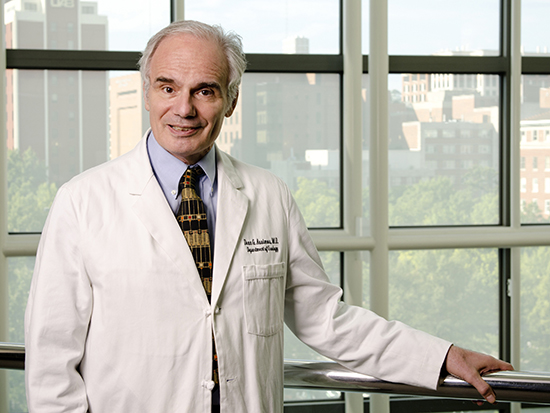
 Dean Assimos, M.D., emeritus professor and founding chair of the Department of Urology at the UAB Heersink School of Medicine, received the 2023 Karl Storz Life Time Achievement Award from the Endourological Society for his contributions to the field of urology.
Dean Assimos, M.D., emeritus professor and founding chair of the Department of Urology at the UAB Heersink School of Medicine, received the 2023 Karl Storz Life Time Achievement Award from the Endourological Society for his contributions to the field of urology.
Kidney stones get no respect — except from anyone who has ever had one. “Kidney stones are the Rodney Dangerfield of diseases,” said Dean Assimos, M.D., emeritus professor and founding chair of the Department of Urology at the UAB Heersink School of Medicine.
You will often hear that kidney stones are more painful than childbirth. That is debatable, although there is this 2017 study from the United Kingdom, in which 12 of 19 female patients who had experienced kidney stones and childbirth rated the stones higher. (Three thought the pain was similar, and four said childbirth was worse.) “They can be excruciating,” confirmed Assimos, who has had two kidney stones himself.
More people than ever are getting that experience. Between 1994 and 2012, the number of Americans with kidney stones nearly doubled. It has now reached one in 10 Americans, “and it is higher in the Southeast,” Assimos said. “About $10 billion a year is consumed taking care of patients with kidney stones and as a consequence of having these patients’ being taken out of the workforce because of the stones.”
Oxalate: a key factor in kidney stones
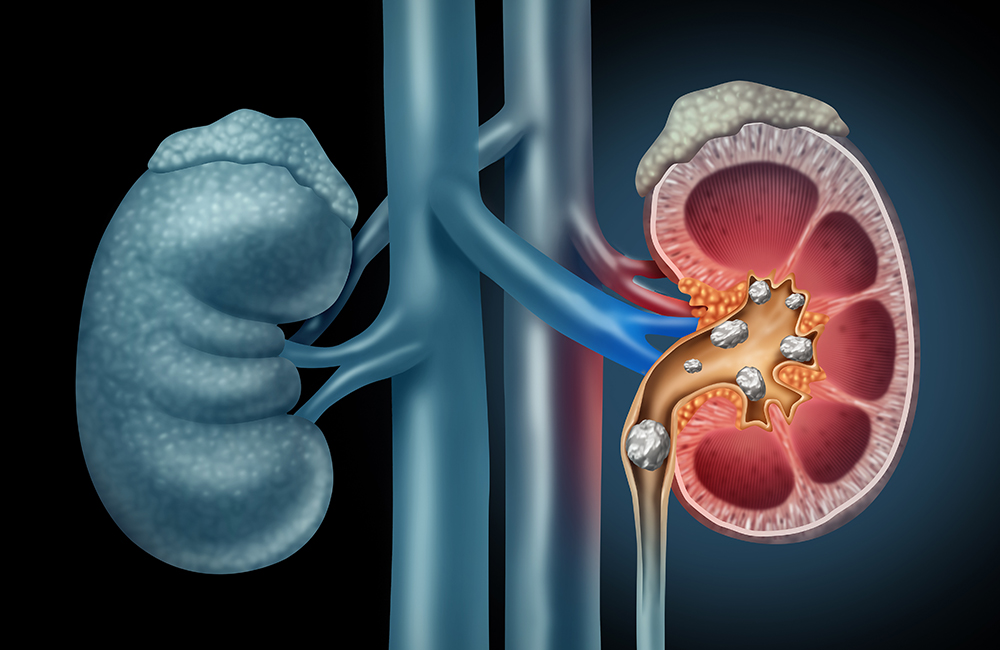
Kidney stones can have multiple causes, but the most common is an accumulation of crystalized oxalate. Oxalate in urine is derived from dietary sources or via the body making it — a process known as endogenous synthesis. Diet-derived oxalate usually binds with calcium in the intestines and leaves the body in the stool in the form of calcium oxalate crystals, Assimos explains. But when there is not enough calcium in the intestinal tract, more of the oxalate remains in its free or soluble form and is readily absorbed from the gut into the bloodstream. It winds up in the kidney, where it is excreted in urine. Oxalate then forms crystals with calcium that accumulates and lodges in the kidney as a stone. (Assimos compares it to how snowflakes stick together to form a snowball.) About 80 percent of kidney stones are composed of calcium oxalate stones, Assimos says. Once you have had one, you are quite likely to have more: The recurrence rate is as high as 50 percent within 10 years.
Assimos has spent his career studying how oxalate is made, handled and excreted by the body, and its effects on kidney stone formation. This work led to his selection for the 2023 Karl Storz Life Time Achievement Award from the Endourological Society for his contributions to the field of urology.
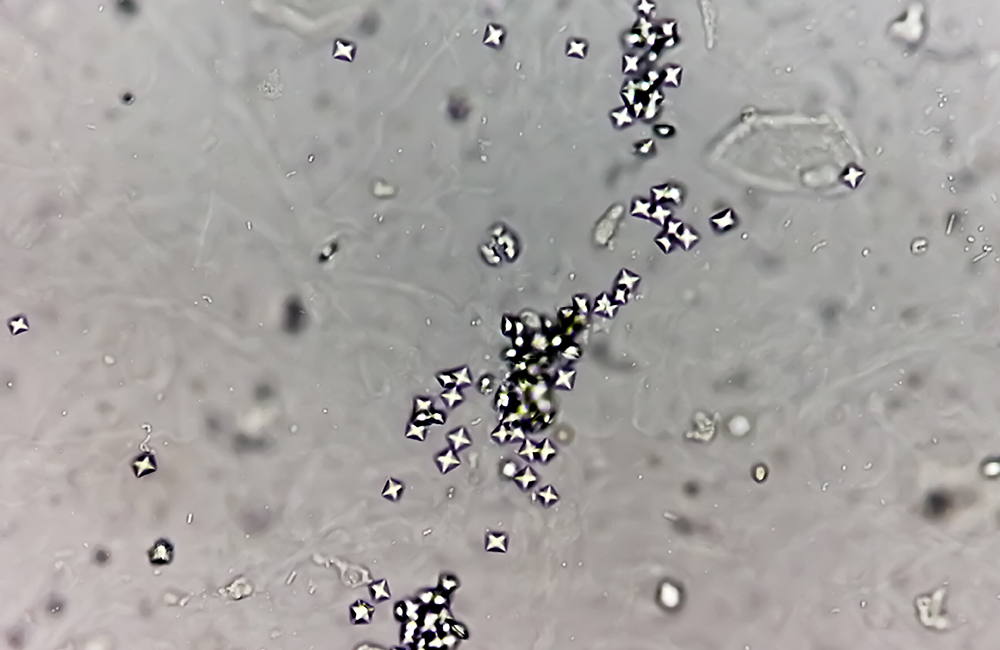 Microscopic image of calcium oxalate crystals
Microscopic image of calcium oxalate crystals
Changes on the horizon
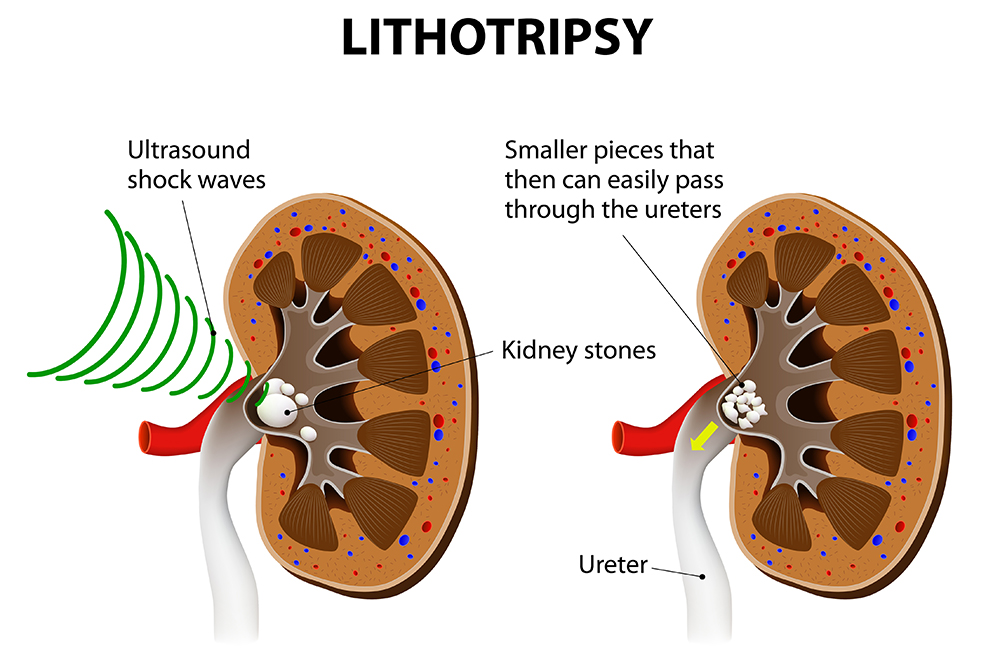
Over the course of his career, Assimos has seen dramatic changes in treatment for kidney stones, and he foresees even more impressive changes just over the horizon. “When I was in training, we were making large incisions to remove stones,” he said. “Now the majority of stones are removed via minimally invasive endoscopy, in which scopes are passed up the ureter to visualize the stone or stones, and they can either be directly removed or broken into small fragments, which are removed or left to pass spontaneously.” Even so, “what we are doing now is still crude,” he said. “I foresee that we will eventually see the development of nano-robots that are programmed to go into the ureter and kidney, where they chip away at the stones and remove them.” Other technology regularly used by urologists to remove kidney stones, including lasers, scopes and extraction devices, will continue to get better and smaller, Assimos predicts.
 "What we are doing now is still crude,” Assimos said. “I foresee that we will eventually see the development of nano-robots that are programmed to go into the ureter and kidney, where they chip away at the stones and remove them."
"What we are doing now is still crude,” Assimos said. “I foresee that we will eventually see the development of nano-robots that are programmed to go into the ureter and kidney, where they chip away at the stones and remove them."Advances in stone prevention: Rare disorders
Efforts at stone prevention are not as far along as stone treatments, Assimos says. The recent advances have come mainly through research into rare genetic diseases that result in heavy stone formation, he explains. One example is primary hyperoxaluria type 1, where the body produces excessive amounts of oxalate that lead to kidney stone formation, oxalate deposition throughout the body and, for many patients, kidney failure. “At one time, the majority who developed kidney failure went on to undergo combined liver/kidney transplantation,” Assimos said. “But medications and methods have now been developed to inhibit enzymes in the liver that influence the production of oxalate.” If the disease is detected before significant kidney damage occurs, “transplantation can be avoided with utilization of these novel treatments, and if not, only renal transplantation may be required,” Assimos said. “Members of the UAB Department of Urology Kidney Stone Research Team have been involved in defining the metabolic derangements associated with increased production of oxalate in this disorder, and other forms of primary hyperoxaluria.”
Cystinuria is another genetic disease associated with the development of cystine kidney stones and chronic kidney disease. Assimos was the first to describe that cystinuria is associated with chronic kidney disease. He predicts that this disease will eventually be cured with a CRISPR-Cas9 gene editing approach targeting the defective cystine transport gene in the proximal tubule of the kidney.
Preventing “garden variety” stones
The majority of those afflicted with kidney stones do not have these rare genetic disorders, Assimos notes. And while dietary modifications and certain medications can be used for stone prevention in the “garden variety” stone former, effective new medications have not been developed, he says. “Stone formation in this cohort may be due to multiple factors, including environment, diet, body composition, socio-economic, demographic, oxidative stress, inflammation, presence of certain medical conditions associated with kidney stone risk and family history,” Assimos said. “The latter infers a genetic risk, which is thought to be due to multiple potentially causative genes, referred to as a polygenic disorder.”
The standard approach to evaluate kidney stone risk has included stone analysis, assessment for medical conditions associated with the development of stones, 24-hour urine stone risk testing, and blood testing to estimate renal function and screen for conditions such as primary hyperparathyroidism and renal tubular acidosis. Assimos predicts that there will be a transition to patients having their mouths swabbed instead for genetic testing. “This will help identify the most effective pathway for stone prevention and targets for drug development,” he said.
Assimos foresees the integration of information on kidney stone risk. “There will be several movements of this informational symphony, including identification of demographic and socioeconomic factors, body composition, indices of inflammation and oxidative stress, stone composition, dietary patterns, targeted blood and urine testing results, assessments of the fecal and urinary microbiome, and gene panels,” Assimos said.
Research on the frontiers of kidney stones
Assimos had already spent the bulk of a distinguished career at Wake Forest University in North Carolina when he was recruited in 2012 by then School of Medicine Dean Ray Watts, M.D., (now UAB’s president) to become the inaugural chair of the UAB Department of Urology. Here he founded the UAB Center for Research on Obesity and Oxalate Kidney Stones, or COOKS, to investigate those looming questions.
“The nice thing about our kidney stone research group at UAB is that they are looking at things from so many directions,” Assimos said.
Diet
COOKS members include Professor Barbara Gower, Ph.D., and Assistant Professor Amy Goss, Ph.D., both faculty in the Department of Nutrition Sciences and scientists in the UAB Nutrition and Obesity Research Center. They lead studies such as a current clinical trial looking at the effects of meal replacement on metabolic function and stone formation. Laura Rogers, M.D., professor in the Division of Preventive Medicine, is a co-investigator of an NIH-funded clinical trial (on which Assimos is the principal investigator) that is assessing the impact of weight loss with a low-calorie dietary program in obese calcium oxalate stone formers. Naim Maalouf, M.D., professor of medicine and associate director of the Charles and Jane Pak Center of Mineral Metabolism at the University of Texas Southwestern School of Medicine, is also a co-investigator on this study and served as a co-investigator of an NIH P20 Center grant focused on obesity and calcium oxalate kidney stone risk, with Assimos as principal investigator.

Microbiome
Associate Professor John Knight, Ph.D., is studying the impact of the gut microbiome on kidney stones, including the effects of gut oxalate-degrading bacteria on urinary oxalate excretion. “There is an organism called Oxalobacter formigenes whose major carbon source is oxalate,” Assimos said. “People can lose colonization with this organism after they take antibiotics, and John has developed a method to re-colonize people and is determining whether this reduces urinary oxalate excretion.”
Endogenous oxalate
Assistant Professor Sonia Fargue, M.D., Ph.D., “is very involved in studying endogenous oxalate synthesis, including the impact of obesity, and doing marvelous work with that,” Assimos said. Knight is a principal investigator of an NIH R01 grant studying the contributions of vitamin C to endogenous oxalate production.
Fatty liver disease
Associate Professor Kyle Wood, M.D., has received an NIH K08 award to investigate the impact of obesity on endogenous oxalate synthesis in animal models. “These animals also develop fatty liver disease, and Kyle is investigating its impact on endogenous oxalate synthesis,” Assimos said. In animal models of severe forms of fatty liver disease, alanine glyoxylate aminotransferase — an enzyme that reduces endogenous oxalate synthesis and is absent or defective in primary hyperoxaluria type 1 — is in lower concentrations in the liver, and this is associated with increased urinary oxalate excretion. “Kyle and Sonia have developed a novel, non-invasive method of assessing the activity of this enzyme, which is very exciting,” Assimos said.
Social determinants of disease
Assistant Professor Joseph Crivelli, M.D., is studying the social and dietary determinants of kidney stone risk in racially and ethnically diverse populations, who bear a disproportionate burden in kidney stone disease. Through an NIH K23 award, Crivelli is leading a clinical trial that will examine the effect of adopting a healthy diet on risk factors associated with kidney stone disease. This will be the first trial of its kind.
Mitochondrial dysfunction
Associate Professor Tanecia Mitchell, Ph.D., is studying the impact of oxalate on mitochondrial dysfunction. Typically, immune cells called monocytes circulate in the bloodstream and, when they land in the kidney, “transition into macrophages, which remove oxalate crystals from the kidney,” Assimos said. “But when a person has mitochondrial dysfunction, that may not happen. That is what Tanecia is investigating.” She was awarded an NIH R01 grant to embark on these studies.
"More gas in the tank"
Assimos stepped down from his chair position in 2022. He was subsequently named emeritus chair and professor and continues to be engaged in research. He has maintained NIH grant support and is a co-principal investigator of a recent NIH-funded U2C-TL1 research training grant. “I’ve had a full career, but I’ve still got gas in the tank,” he said. “Some urologists spend a lot of time looking at devices to facilitate stone removal. I’ve done a little bit of that, but it’s not what drives me. It doesn’t tell you what you need to know about the disease.”
Preventing stones
Kidney stones are caused by a complex mix of genetic, environmental and dietary factors; but there are several ways you can reduce your risk, says kidney stone expert Dean Assimos, M.D., emeritus chair and professor in the UAB Department of Urology.
1. Drink plenty of water.
Dehydration is a key risk factor for stones. Drink at least six to eight glasses of fluid a day — and more when you are exposed to extreme heat.
2. Get calcium from food sources.
Even though most stones are caused by excess calcium in the urine, calcium consumption is a good thing. Research shows that dietary calcium binds to oxalate, limiting its absorption from the gastrointestinal tract and delivery to the kidney. Low dietary calcium intake has been demonstrated to be a risk factor for kidney stones in several large epidemiologic cohort studies. Thus, try to eat one serving of dairy products with each meal, Assimos says. However, calcium supplements do not offer the same benefits; in fact, they appear to increase stone risk.
3. Eat less animal protein and salt.
Animal protein and salt (sodium) boost calcium excretion in urine, increasing the risk of forming calcium-containing kidney stones.
4. Stock up on citrus.
Citric acid, found in oranges and other citrus fruits, inhibits some of the crystallization processes involved in stone formation; eating citrus may reduce stone formation.
Assimos says that dietary modifications to prevent kidney stone formation are based on consuming a healthy diet.