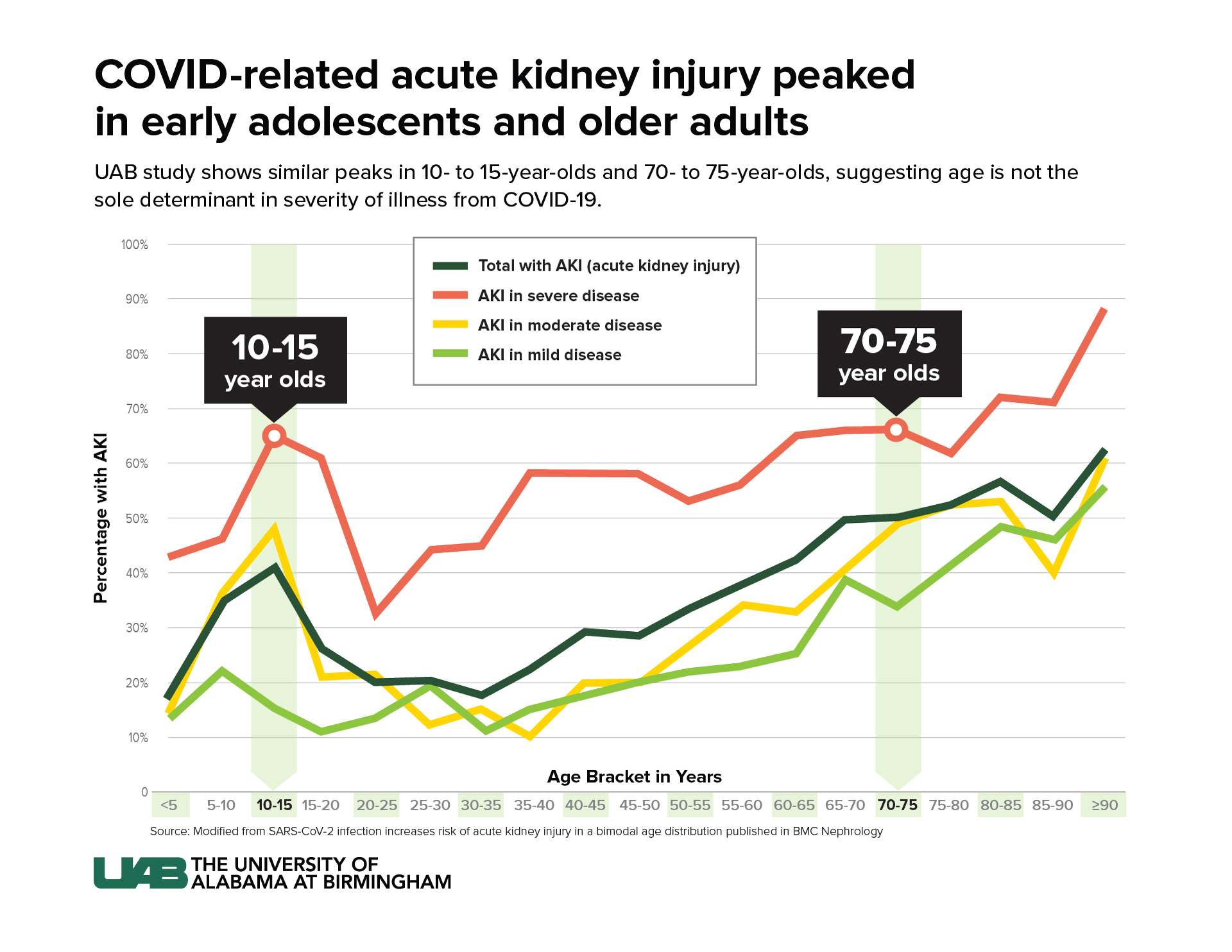
 Graphic: Jody PotterAcute kidney injury is increasingly recognized as a significant complication caused by COVID-19 infection. Researchers from the University of Alabama at Birmingham and Children’s of Alabama studied the epidemiology of coronavirus-related AKI and discovered peaks in AKI in early adolescents and adults older than 60.
Graphic: Jody PotterAcute kidney injury is increasingly recognized as a significant complication caused by COVID-19 infection. Researchers from the University of Alabama at Birmingham and Children’s of Alabama studied the epidemiology of coronavirus-related AKI and discovered peaks in AKI in early adolescents and adults older than 60.
“Since the beginning of the pandemic, there has been the assumption that the severity of COVID-19 related illness is linear with age — the older one is, the more at risk they are for severe illness,” said Erica Bjornstad, M.D., Ph.D., assistant professor in the UAB Marnix E. Heersink School of Medicine and Children’s Division of Pediatric Nephrology. “Our findings indicated increased risk in both early adolescents and older adults, suggesting factors besides age could be determinants in severity of illness from infection.”
The observational study, recently published in BMC Nephrology, used the Viral Infection and Respiratory Illness Universal Study initiated by the Society of Critical Care Medicine in January 2020. The analysis included patients admitted between January 2020 to March 2021. Of the 6,974 patients, 39.6 percent developed AKI within the first seven days of hospitalization. Among those younger than 20 years of age, 28 percent developed AKI.
AKI, a sudden episode of kidney damage or failure, can cause buildup of waste products in the bloodstream and makes it harder for kidneys to balance bodily fluids. Symptoms from AKI range from a decrease in urine output, swelling and fatigue to seizures and coma and require dialysis in severe cases. The risk of developing chronic kidney disease and kidney failure increases every time an AKI occurs, according to the National Kidney Foundation.
The specific cause of COVID-related AKI is still unknown. Some cases may be caused by typical risk factors of AKI, such as critical illness and dehydration. However, after evaluating the pattern of AKI related to age, the research team theorizes there may be additional causes in COVID-related AKI. The age distribution suggests there could be a combination of COVID-related diseases that affect blood vessels along with hormonal influences. The virus has a propensity to attack endothelium tissue, which lines blood and lymphatic vessels. Damage to the endothelium can cause a sudden drop in blood flow, which can cause AKI.
“In older adults, endothelium tissue ages and is more prone to damage,” Bjornstad said. “As for early adolescents, the team believes it is possible that a hormonal influence leads to a higher chance for endothelium damage, but the exact reason for the peaks of COVID-related AKI in adolescents and older adults needs further study.”
Analysis consistently showed the odds of developing COVID-related AKI were similar for early adolescents ages 10 to 15, as well as adults between 70 and 75 years of age, increasing 2.5-fold over young adults ages 30 to 35. The pattern remained after adjustments for other potential variables such as comorbidities, preexisting conditions, sex, race and ethnicity. The same pattern also occurred when participants were categorized into severe, moderate and mild coronavirus infection.
Bjornstad also notes there are unknown biological mechanisms that could contribute to the pattern of increased risk in adolescents and older adults as the study could not account for different strains of coronavirus in participants. However, their findings are one of many studies that reiterate COVID-related AKI at any stage increases patients’ morbidity and mortality.
“More in-depth exploration is needed to fully understand the age pattern found in our study,” Bjornstad said. “As the pandemic lingers, outbreaks continue and younger children remain unvaccinated, it is important to understand this age phenomenon — whether it is biologically based or caused by certain risk factors — to help guide clinical care improvements in COVID-related AKI.”
The study is supported by the Society of Critical Care Medicine with partial funding from Gordon and Betty Moore Foundation and Janssen Research & Development, LLC.