A novel type of multi-functional, cyto-protective material developed by University of Alabama at Birmingham researchers allows pancreatic islets in mice and humans to maintain viability and ?-cell functionality for at least 96 hours in vitro. The ultrathin polymeric coating, based on hydrogen-bonded polyphenol, also demonstrates the ability to modulate pro-inflammatory cytokine synthesis, according to a study published in the online edition of Advanced Functional Materials.
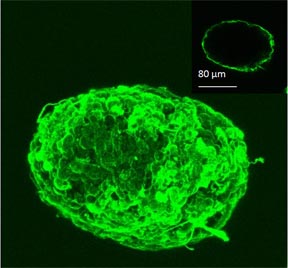 |
| Coated islet cross section |
Islets, known as the Islets of Langerhans, are clusters of cells in the pancreas that release insulin that enables the human body to maintain normal blood-sugar levels. There are an estimated 1 million islets in an adult pancreas, but they make up only 1 percent to 2 percent of the entire organ. These are the cells that are attacked in Type 1 diabetes.
“This eventually could lead to a new way to treat diabetes that would require only one initial surgery to transplant healthy pancreatic islets into the patient and replace the need for lifelong daily insulin injections,” says Eugenia Kharlampieva, Ph.D., assistant professor in the Department of Chemistry and lead author of the study. “The coating is nano-thin so it does not increase the volume of the islets. It is permeable so the islets receive nutrients and secrete insulin, and the coating is friendly so it doesn’t kill the cells.”
Other researchers’ previous attempts to extend the lives and retain functionality placed the islets in thick hydrogels. The UAB team, however, developed a layer-by-layer method by which individual polymer coatings are placed on top of each other much like stacking pancakes. Each layer is 2 to 4 nanometers thick with the optimal goal being a coating that is 20-40 nanometers thick. This approach allows the researchers to control the thickness and the behavior of the polymers.
“The advantage of our technology is that our polymers are not charged so they do not have the electrostatic drive to penetrate the membrane, which would eventually kill the cell,” says Kharlampieva. “These neutral polymers are neutral and bio-compatible and can interact with the membrane by hydrogen-bonding interaction, which allows layers to be stacked and retain permeability.”
The work is a collaboration between UAB’s College of Arts and Sciences and School of Medicine. Co-authors include Hubert Tse, Ph.D., from the Department of Microbiology, and Anthony Thompson, Ph.D., professor of surgery, director, Division of Transplantation Research and Development. Their research was specific to the viability and functionality of the islets, but they found another unique feature of their polymers in the process. The pancreatic islets, once coated with the polymer, have a tremendous immuno-modulatory response.
“We found that our islet-coating material could induce an anti-inflammatory response with macrophages and auto-reactive T cells that contribute to transplantation rejection,” said Tse. “We still need to define the mechanisms involved in the immuno-modulatory response with these unique polymers, but as we move toward in vivo research, we are all excited about the potential to change how we treat the millions suffering from diabetes.”