 Maria Danila, M.D. According to the Centers for Disease Control and Prevention, approximately 24 percent of adults in the United States have some form of arthritis, an autoimmune disease that causes painful inflammation, typically in joints. Early diagnosis of rheumatoid arthritis can significantly reduce the risk of joint damage, functional impairment and pain — all issues that can impact one’s daily life.
Maria Danila, M.D. According to the Centers for Disease Control and Prevention, approximately 24 percent of adults in the United States have some form of arthritis, an autoimmune disease that causes painful inflammation, typically in joints. Early diagnosis of rheumatoid arthritis can significantly reduce the risk of joint damage, functional impairment and pain — all issues that can impact one’s daily life.
Diagnosing arthritis begins with a history and physical examination looking for signs of inflammation: swollen joints, joint stiffness, joint pain and tenderness, and a decrease in range of motion. However, since not all signs of arthritis are visible to the naked eye, making accurate diagnosis of arthritis during telemedicine visits represents a challenge.
Rheumatologists from the University of Alabama at Birmingham Marnix E. Heersink School of Medicine are looking to bridge this information gap by incorporating imaging using thermography cameras into telemedicine visits. The forward-looking infrared cameras use infrared radiation to provide detailed images of inflamed areas, thus assisting in diagnosis of arthritis.
“Studies have shown that telemedicine visits can expand the access to rheumatology care for those living in rural areas with limited access to such specialized health care services,” said Maria Danila, M.D., associate professor in the UAB Division of Clinical Immunology and Rheumatology, scientist with the Birmingham/Atlanta Veterans Affair Geriatric Research Education and Clinical Center, and project lead. “Quickly and accurately diagnosing arthritis can be difficult during telemedicine visits due to the limitations in physical examination inherent to virtual visits. Infrared thermographic imaging may help detect joint inflammation, thus providing us with additional key information to enable us to deliver appropriate rheumatology care.”
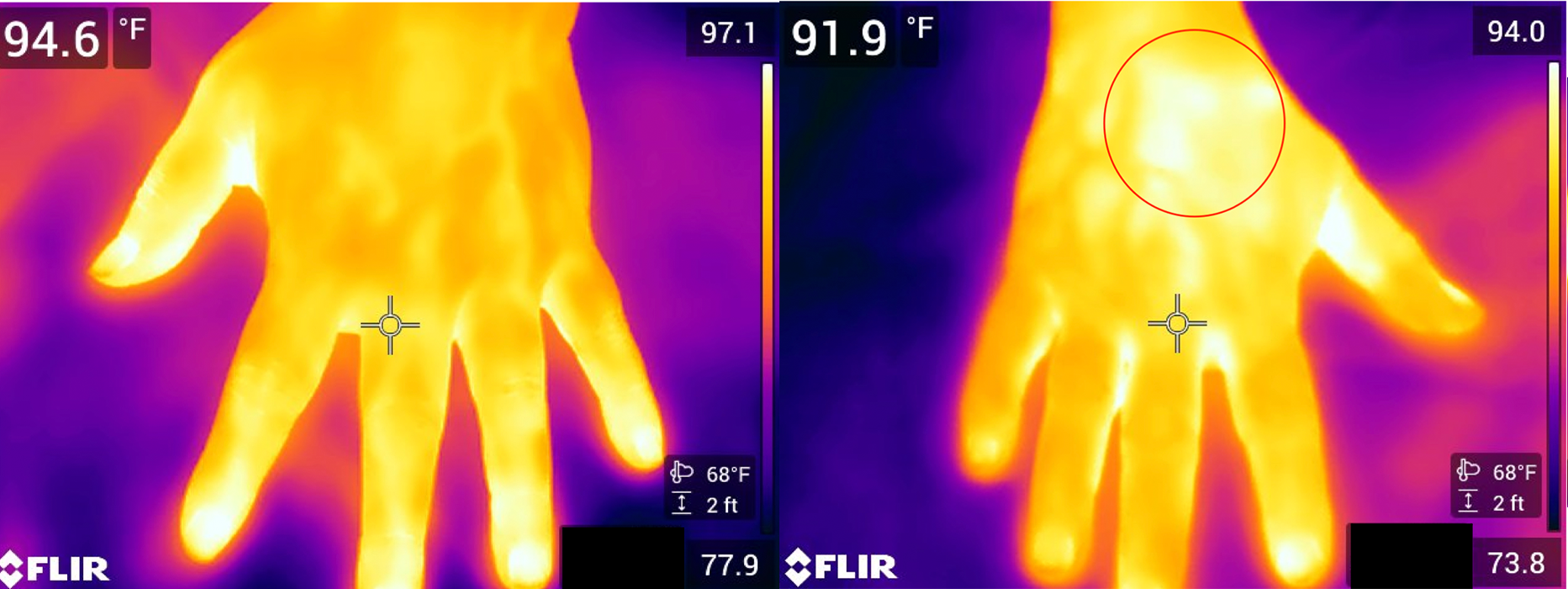 Image on the left shows no inflammation. Circled area on the right image shows inflammation.Through a grant funded by Pfizer, Inc., Danila and her UAB research team will first optimize protocols for infrared thermography using musculoskeletal ultrasound as the standard. The team will then train nursing staff at Whitfield Regional Hospital in Demopolis, Alabama, and John Paul Jones Hospital in Camden, Alabama, both members of the UAB Health System, on how to use the cameras to obtain images of a patient’s hands and feet.
Image on the left shows no inflammation. Circled area on the right image shows inflammation.Through a grant funded by Pfizer, Inc., Danila and her UAB research team will first optimize protocols for infrared thermography using musculoskeletal ultrasound as the standard. The team will then train nursing staff at Whitfield Regional Hospital in Demopolis, Alabama, and John Paul Jones Hospital in Camden, Alabama, both members of the UAB Health System, on how to use the cameras to obtain images of a patient’s hands and feet.
Images will be sent to UAB rheumatology clinicians who provide consultative care through telemedicine. The team will test whether the infrared thermography imaging can be effectively implemented to enable remote examination for joint inflammation.
“Many Alabama residents live in rural areas where access to specialized care, such as that provided by rheumatologists, is limited,” Danila said. “We hope this new technology will help eliminate some of the health care barriers our rural rheumatology patients experience.”