Media contact: Bob Shepard
 AGHI is one of the nation’s first statewide efforts to harness the power of genomic analysis to find answers for those with undiagnosed developmental and medical challenges.Some of the first results from the Alabama Genomic Health Initiative were recently published in Genetics in Medicine. The AGHI, launched in 2017, is one of the nation’s first statewide efforts to harness the power of genomic analysis to find answers for children and adults with undiagnosed developmental and medical challenges, and to identify individuals who are at a higher risk for developing certain diseases in the future.
AGHI is one of the nation’s first statewide efforts to harness the power of genomic analysis to find answers for those with undiagnosed developmental and medical challenges.Some of the first results from the Alabama Genomic Health Initiative were recently published in Genetics in Medicine. The AGHI, launched in 2017, is one of the nation’s first statewide efforts to harness the power of genomic analysis to find answers for children and adults with undiagnosed developmental and medical challenges, and to identify individuals who are at a higher risk for developing certain diseases in the future.
The program is a collaboration between the HudsonAlpha Institute for Biotechnology and the University of Alabama at Birmingham, funded by the state of Alabama. It is led by Bruce Korf, M.D., Ph.D., chief genomics officer at UAB; Greg Barsh, M.D., Ph.D., faculty chair and senior scientist at HudsonAlpha; and Matthew Might, Ph.D., director, and Nita Limdi, Pharm.D., Ph.D., associate director, of the Hugh Kaul Precision Medicine Institute at UAB.
AGHI provides genomic testing, interpretation and counseling free of charge to Alabama residents. The goal of the program is to engage at least 10,000 Alabamians in genetic testing, while educating the participants about their genomic health.
“AGHI is helping to improve patient care, not only by providing diagnoses, but also by giving the general public a foundational understanding of the importance and value of being informed about their genomic health,” Barsh said. “Through the AGHI platform, we are able to provide an invaluable opportunity to physicians and geneticists to confirm or identify a diagnosis that has gone undiagnosed despite a vast array of previous medical testing.”
“The rise in the availability and affordability of clinical genomic testing has done wonders for rare disease diagnosis,” Korf said. “Genomic sequencing has been well-established as a useful diagnostic tool for patients with rare genetic diseases. However, access to genomic testing, and the knowledge of its usefulness in diagnosing and predicting disease, is not widely available throughout our country.”
AGHI engages two distinct groups of participants across the state of Alabama: children and adults with undiagnosed rare disease, and adults in the general population who do not have a significant personal or family history suggestive of a genetic condition. The published data reflects the first 176 rare-disease participants and 5,369 participants in the population screening group.
Participants were recruited at sites across the state, including locations in Madison, Jefferson, Montgomery, Mobile and Baldwin counties. They provided a small sample of blood as well as information about their personal and family health history. DNA was extracted from the blood sample and analyzed. Participants in the population screening group received a genotyping test, while participants in the rare-disease group received genome sequencing. Genotyping tests look at a preselected group of variants that are known to increase a person’s likelihood of disease, while whole-genome sequencing looks at every single letter of the genetic code. (Learn more about the differences in genotyping and genome sequencing here.)
All participants received a report summarizing the results of their tests. Individuals whose results include actionable findings received genetic counseling and a referral to appropriate medical care.
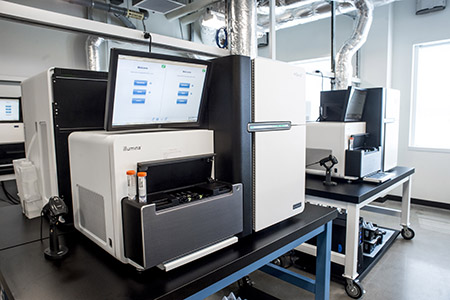 Genetic sequencing equipment at HudsonAlpha can be used to look for genetic variants that may contribute to disease.“We speak by phone with participants who have an identified genetic risk factor,” said co-author Whitley Kelley, a genetic counselor at HudsonAlpha. “During these conversations, we explain what it means to have a genetic risk factor using clear language, in contrast to some of the more technical data that may be included on their result report. Then we provide recommendations for clinical resources that can guide their next steps in prevention and personalized health management. It is important to us to make sure the participants understand their results and the implications of those results, both for themselves and for their family members.”
Genetic sequencing equipment at HudsonAlpha can be used to look for genetic variants that may contribute to disease.“We speak by phone with participants who have an identified genetic risk factor,” said co-author Whitley Kelley, a genetic counselor at HudsonAlpha. “During these conversations, we explain what it means to have a genetic risk factor using clear language, in contrast to some of the more technical data that may be included on their result report. Then we provide recommendations for clinical resources that can guide their next steps in prevention and personalized health management. It is important to us to make sure the participants understand their results and the implications of those results, both for themselves and for their family members.”
In the rare-disease group, of the 176 affected individuals, 35 (19.9 percent) received a pathogenic or likely pathogenic result, meaning a genetic variant was found that is believed to contribute to disease. In addition, 42 individuals (23.9 percent) received an uncertain result, meaning a genetic variant was found that is not well understood, but may contribute to disease. The new genetic knowledge, combined with the individual’s symptoms, often allows doctors to make a diagnosis for a disease that had remained undiscovered for months or years.
“Being able to provide answers to individuals and their families who have been impacted by rare disease who may not have been able to otherwise access genome sequencing is one of the crowning achievements of AGHI to date,” said co-author Kelly East, a genetic counselor at HudsonAlpha. “We hope that the AGHI model can help inform similar programs elsewhere to give more communities awareness of and access to genomic testing.”
To date, 5,369 individuals, representing all 67 Alabama counties, have been enrolled in the population screening group of AGHI. Eighty-one positive genotyping results among 80 individuals (1.5 percent) were identified in the population cohort. These results include risk-increasing variants for hereditary cancer, cardiomyopathy, malignant hyperthermia and hypercholesterolemia. These results were expounded upon in a corresponding publication in Genetics in Medicine that highlight findings on the effectiveness of population-based genomic screening.