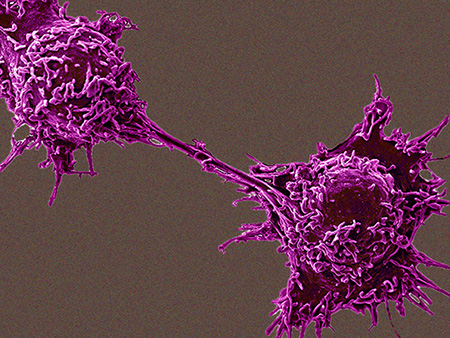
 A study identifying biomarkers for certain neuroendocrine cancers demonstrates a novel approach for identifying and detecting tumor drivers, giving this diagnostic-therapeutic coupled system a broad translational potential.Precision medicine in cancer treatment uses genetic changes in the cancer cells to select the best therapies for individual patients.
A study identifying biomarkers for certain neuroendocrine cancers demonstrates a novel approach for identifying and detecting tumor drivers, giving this diagnostic-therapeutic coupled system a broad translational potential.Precision medicine in cancer treatment uses genetic changes in the cancer cells to select the best therapies for individual patients.
Now researchers led by James Bibb, Ph.D., professor of surgery at the University of Alabama at Birmingham, suggest using a broader lens of post-translational modification analysis to identify new biomarkers of cancer drivers that may allow a much more precise prediction of patient responses to treatments. In a study published in Proceedings of the National Academy of Sciences, they demonstrate this diagnostic alternative for neuroendocrine neoplasms driven by an aberrantly activated protein kinase called Cdk5.
“Our findings show that precision medicine is a realizable goal for the treatment of rare and recalcitrant cancers,” said Angela Carter, Ph.D., principle author of the paper and a postdoctoral fellow in the Bibb lab at UAB.
“The same approach,” Bibb said, “could be adapted to identify markers of other tumor drivers. As the number of cancer types in which Cdk5 is implicated is rising, and as drugs with the potential to selectively target Cdk5 are moved toward the clinic, the translational potential of this diagnostic-therapeutic coupled system will be broad.”
UAB researchers are now in collaboration with the National Cancer Institute to adapt the biomarkers the team discovered into a clinically applicable diagnostic assay, and move new drugs targeting these pathways to clinical trials.
Cdk5 is a cyclin-dependent kinase that phosphorylates target proteins as part of signaling sequences in cells. Cdk5 activity is mostly restricted to neuronal cells, where it is important for central nervous system development and cognitive processes such as learning and memory.
In the PNAS paper, Carter, Bibb and colleagues first examined multiple samples of neuroendocrine tumor and cancer types and found that Cdk5 and its activators p35 and p25 characterized a large portion of all neuroendocrine neoplasms. Also, a Cdk5 inhibitor blocked growth of the neoplasms, showing that Cdk5 activity is a major contributor to the growth of these cancer cells.
To find biomarkers, the researchers first used a unique mouse model of medullary thyroid carcinoma, or MTC, whose growth of the tumor can be turned on or off. They then looked for global differences in phosphorylated peptide fragments between arrested and growing MTC. The 50 most highly upregulated phosphorylation sites in growing MTC were examined further, using short interfering peptides that would block phosphorylation. Fifteen interfering peptides were found to inhibit growth of neuroendocrine cancer cells but not normal fibroblasts, which identified the downstream targets of Cdk5 needed for cancer cell growth. The 15 targets of the Cdk5 signaling cascade were shown to come from proteins associated with common cancer mechanisms.
Phosphorylation state-specific antibodies were generated to detect six of those sites and two other sites previously identified as targets of Cdk5. Six of the eight sites showed dose-dependent reduction by a Cdk5 inhibitor in a human neuroendocrine cancer cell line, meaning decreased phosphorylation of the proteins the peptides came from. “Our overall data demonstrated that phosphorylation of these six proteins is critical in driving these cancers and is dependent upon Cdk5 activity. It also suggested that these phosphorylation sites could serve as biomarkers for many types of Cdk5-driven neuroendocrine tumors,” Bibb said.
Three showed significant elevation in a cohort of human MTC patient tumors and a positive correlation with Cdk5 expression; another was increased in just a small portion of tumor samples but had a positive correlation with Cdk5 expression. Nearly three-fourths of patient tumors tested showed elevated Cdk5 levels; but only one-fifth had elevation of all four biomarkers of Cdk5 pathway activity, emphasizing that presence of a protein does not correlate completely with function of that protein.
The researchers then showed that Cdk5 inhibition blocked the growth of tumors in distinct MTC animal models. They then tested patient-derived xenograft models for presence of the putative Cdk5 biomarkers, and showed that growth of two biomarker-positive cancers was reduced by treatment with the Cdk5 inhibitor, while tumor growth of the two biomarker-negative cancers was not. These results strongly supported the ability of the biomarkers to predict responsiveness to anti-Cdk5 therapy.
 James Bibb, Ph.D., professor of surgery However, tumor regression was not seen, and higher levels of the Cdk5 inhibitor were quite toxic. So the researchers tested a biomimetic nanoparticle-based drug delivery system called leukosomes, or LKs, which were generated from a combination of synthetic phospholipids and leukocyte membrane extracts. LKs have the ability to target the inflamed environment of a tumor, and their leukocyte membrane proteins camouflage them from removal by the immune system.
James Bibb, Ph.D., professor of surgery However, tumor regression was not seen, and higher levels of the Cdk5 inhibitor were quite toxic. So the researchers tested a biomimetic nanoparticle-based drug delivery system called leukosomes, or LKs, which were generated from a combination of synthetic phospholipids and leukocyte membrane extracts. LKs have the ability to target the inflamed environment of a tumor, and their leukocyte membrane proteins camouflage them from removal by the immune system.
The LKs showed increased localization at MTC tumors in mice, where they could deliver a lower dose of the Cdk5 inhibitor that had the same effectiveness as a higher, toxic dose of free Cdk5 inhibitor.
“The current study reveals that Cdk5 is likely a contributor to at least a portion of all neuroendocrine tumor types,” Bibb said. “This study also identifies a set of phosphorylation-based biomarkers, which indicate that not only are Cdk5 pathway components present, but Cdk5 is actively modulating the signaling network and regulating cancer physiology.
“To be useful clinically, antibodies to detect these biomarkers will need to be developed into an easy-to-use assay that allows reliable quantitation of biomarker levels in patient tumors, preferably in relatively small samples such as core biopsies.”
UAB co-authors with Bibb and Carter in the study, “Phosphoprotein-based biomarkers as predictors for cancer therapy,” are Rahul Telange, Sushanth Reddy, Renata Jaskula-Sztul and Herbert Chen, UAB Department of Surgery; Nileh Kumar and Shahid Mukhtar, UAB Department of Biology; and James Mobley, UAB Department of Anesthesiology and Perioperative Medicine.
Reddy and Jaskula-Sztul are associate scientists, and Chen and Bibb are senior scientists, in the O’Neal Comprehensive Cancer Center at UAB.
The international effort also received collaborative contributions from numerous institutes, including M.D. Anderson Cancer Center, Cell Signaling Technology, Houston Methodist Hospital, the Eunice Kennedy Shriver National Institute of Child Health, Boehringer Ingelheim, and the University of Sydney, Australia.
Support came from the American Cancer Society, the North American Neuroendocrine Tumor Society, the SDHB Pheo/Para Coalition and the O’Neal Comprehensive Cancer Center at UAB.
Bibb is vice chair for Basic Research in the Department of Surgery at UAB, and he holds the
Dr. Champ Lyons Endowed Chair in General Surgery.