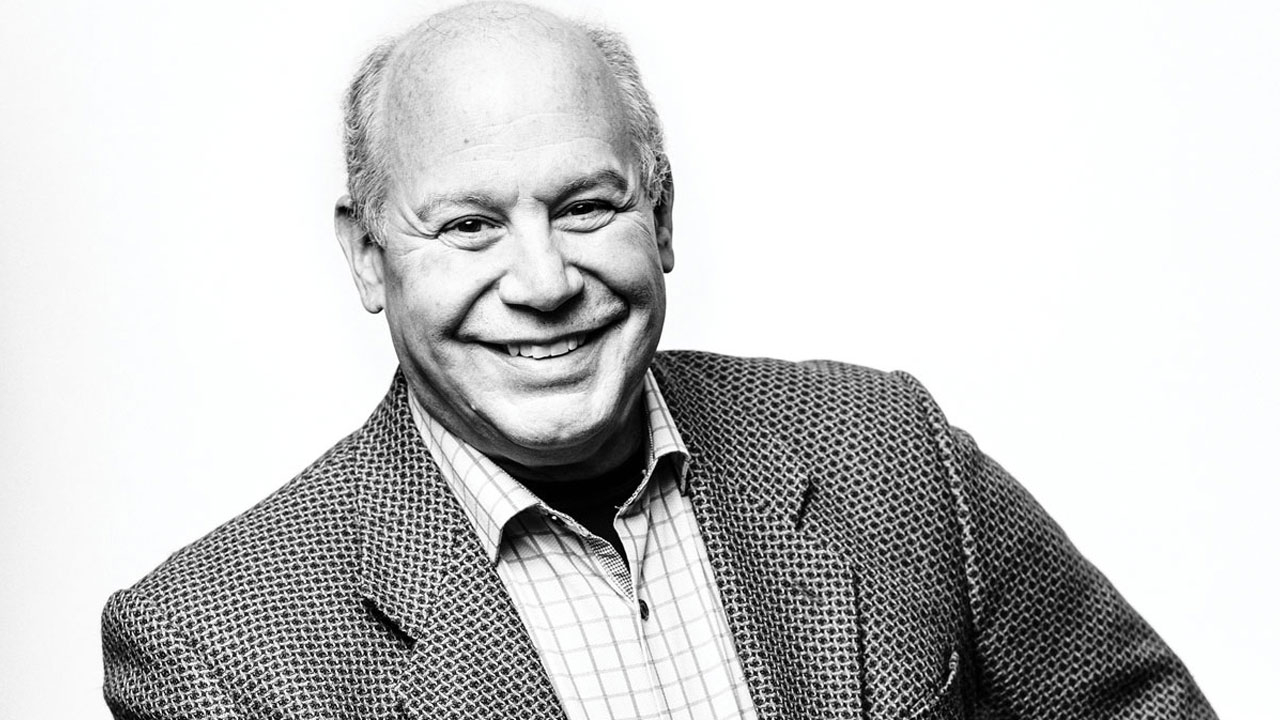
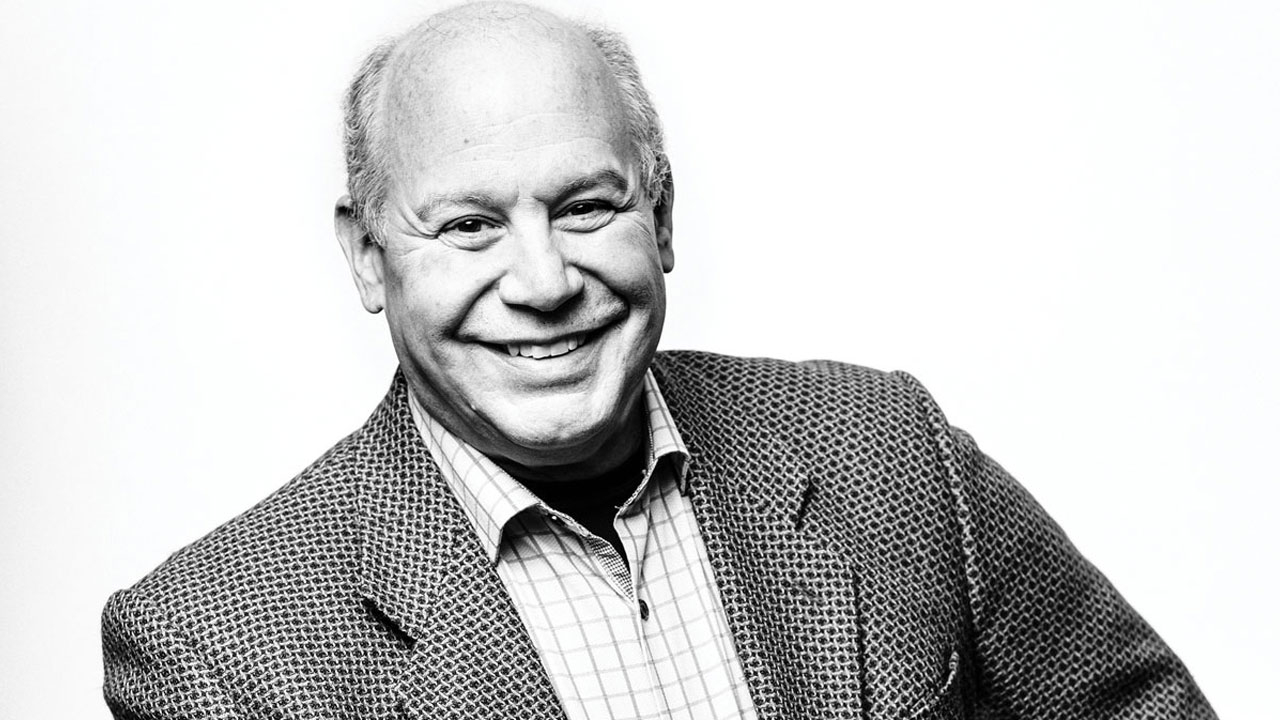
IN 2021, MICHAEL SAAG, M.D., RETIRED FROM UAB—just over 40 years to the day after arriving in Birmingham for his internal medicine residency. He remains a professor emeritus in medicine, microbiology and public health, and a legend in the field of HIV/AIDS, where he is an editor of the top journal, a member of the Presidential Advisory Council of HIV/AIDS, and the recipient of research grants surpassing $100 million. Saag will continue to see patients and run one of his grants, CNICS, which is a project of the UAB Center for AIDS Research. Saag is a founding co-director of that center, one of the first seven CFARs established by the NIH in 1988. In the same year, he founded the UAB AIDS (1917) Outpatient Clinic, the first HIV clinic in the State of Alabama.
MATT WINDSOR: How did UAB become a leader in HIV/AIDS research and care?
MIKE SAAG: “It was a great confluence, with people coming together at the right place and right time with the right resources. Eric Hunter, the founding director of the CFAR, was already here, and he was a retrovirologist before HIV—which is a retrovirus—came along. In 1985, GeorgeShaw and Beatrice Hahn moved here from the Gallo Lab [at NIH, which had discovered HIV as the cause of AIDS], and I was just coming out of residency. And UAB itself, the leadership and administration, was extremely supportive; not too different from how we came together to fight COVID and take a leadership role there. The difference being that COVID doesn’t carry universities didn’t want anythingto do with HIV. They thought it would hurt the reputation of their hospitals if they had HIV patients there.”
MW: You have made numerous contributions as a researcher. Which ones stand out for you?
MS: “The initial one happened when I was a fellow. We described the ‘quasi-species’ nature of HIV. Once someone is infected with a random variant, it mutates very rapidly to escape the immune response. We stumbled onto this fact with genetic analysis. We found that as many as 20 to 30 different variants were circulating simultaneously. The virus would escape, and the immune system had to chase after it. “The second discovery was the use of viral load, which we now use all the time. One of the mysteries early on was why there was aninitial peak viral load (amount of HIV) in the blood, which seemed to go away for years and then come back again. The assumption was that the virus was initially replicating, then it was shut down, and then as the patient got sick, the virus would come back. But in 1992, we found that viral replication was continuous and never really went away. There was ongoing replication, and over time, it eroded the immune system’s ability to function properly. This discovery revealed the primary reason (relentless, persistent viral replication) people got sick and died from HIV. “We also saw that viral load measurement was a tool we could use to track the response to antiviral drugs in every patient. This allowed us to determine, within days to weeks, if the drugs worked. If they did, we saw a sudden drop in viral load. That discovery alone saved enormous numbers of lives because we didn’t have to wait for clinical endpoints (e.g., body counts) to determine that a drug worked. This brought in most of the pharmaceutical companies to UAB, right as a lot of new drugs were being developed in the early 1990s. We became one of the epicenters of drug discovery. That is why we were the first in the world to use the ‘HIV cocktail,’ the triple drug therapy.”
MW: Tell me how you came to start the 1917 Clinic.
MS: “In December 1986, I went to UCSF and gave a lecture on genetic variation in HIV. They started the world’s first HIV outpatient clinic in 1981. I asked all their top clinicians and researchers one question: ‘If you were starting over, what would you do differently?’ I took those lessons back andwent to Claude Bennett, who was chair of Medicine at the time. Four minutes into my presentation, he said, “Stop. This is a great idea. We’ll bring you on as faculty and give you start up money and space.” At the time I thought this was normal, but later I realized that many institutions responded in exactly the opposite way. And few institutions would invest in the vision set forth from a young person still in fellowship training. That is what made UAB so special for me.”
MW: What are the major HIV/AIDS questions that still need to be answered?
MS: “Overall, the challenge is how do we end the HIV epidemic. That requires a marked reduction in transmission over time and will require reaching populations at risk and intervening before they have an exposure or minimizing exposures. Ultimately, of course, having a vaccine and a cure are long-term objectives. At the present time, we control HIV just like [we control] diabetes with insulin, but we don’t eliminate it. It exists in cellular reservoirs that persist for life. If we could get rid of those reservoirs, people would be cured.”