 Despite decades of research and billions of dollars in pharmaceutical development, many psychiatric disorders have proved stubbornly resistant to treatment. Depression, one of the most common psychiatric disorders, affects 5 percent of adults worldwide, or approximately 280 million people. Annually, 7.1 percent of American adults will have a major depressive episode, and half of those will receive medication treatment. But many will not find relief. In a 2021 study, researchers estimated that more than 30 percent of the 8.9 million American adults being treated with medication for major depressive disorder have treatment-resistant depression, defined as failing to respond or achieve remission after two or more trials of medication treatment.
Despite decades of research and billions of dollars in pharmaceutical development, many psychiatric disorders have proved stubbornly resistant to treatment. Depression, one of the most common psychiatric disorders, affects 5 percent of adults worldwide, or approximately 280 million people. Annually, 7.1 percent of American adults will have a major depressive episode, and half of those will receive medication treatment. But many will not find relief. In a 2021 study, researchers estimated that more than 30 percent of the 8.9 million American adults being treated with medication for major depressive disorder have treatment-resistant depression, defined as failing to respond or achieve remission after two or more trials of medication treatment.
Depression treatments, along with medications for other psychiatric disorders, are primarily designed to target neurons and neurotransmitters. But neurons are not the only cells in the brain. In fact, astrocytes are somewhat more numerous cells in this space. They are a subtype of cells known as glia that are found in the brain, spinal cord and peripheral ganglia and act to keep the brain in homeostasis at the organ, tissue, cell and molecular levels, says Vladimir Parpura, M.D., Ph.D., professor in the Department of Neurobiology. “Brain homeostasis lies at the fulcrum of healthy brain function, and compromise of that homeostasis inevitably results in disease,” Parpura said.
Mood disorders, schizophrenia, addictive disorders, eating disorders
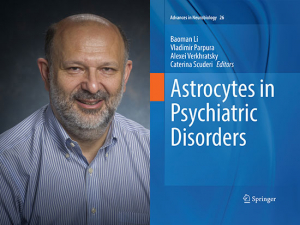
Parpura and colleagues recently published “Astrocytes in Psychiatric Disorders,” a first-of-its-kind book that reviews the cutting-edge research around the roles of these cells in mood disorders, schizophrenia, addictive disorders and eating disorders. The book also explores methods of targeting astrocytes in the therapeutic management of neuropsychiatric disorders. “Multiple roles of astrocytes, which determine the progression and outcome of neuropsychiatric diseases, are emerging,” Parpura said. “It is becoming clear that astrocytes are involved in various aspects of disease initiation, progression and resolution. In this monograph, we aimed to integrate the body of information that has accumulated in recent years that reveals the active role of astrocytes in neuropsychiatric pathology. Understanding the roles of astrocytes in pathology will provide new targets for medical intervention and aid the development of much-needed therapeutics.”
“Multiple roles of astrocytes, which determine the progression and outcome of neuropsychiatric diseases, are emerging. It is becoming clear that astrocytes are involved in various aspects of disease initiation, progression and resolution.”
Astrocytes possess transporters and receptors for a variety of neurotransmitters, which would allow them to be a target for therapeutics, Parpura says. And many existing medications may rely for their effects in part on their manipulation of astrocytes. In animal models of major depressive disorder, there is evidence that astroglial receptors, in addition to receptors on neurons, are targeted by the widely used depression medications known as SSRIs and SNRIs, for example.
Parpura himself discovered in the early 1990s that astrocytes can release glutamate, which is a major neurotransmitter, using exocytosis to signal to nearby neurons. (That discovery, documented in a landmark paper in Nature in 1994, has resulted in Parpura’s selection as a 2017 Fellow of the American Association for the Advancement of Science, among other honors.)
Astrocytes responding to stress and injury
In general, glial cells have three levels of response to stress or injury, two of which play roles in neuropsychiatric disorders, Parpura says. The first is reactive astrogliosis, which “is basically a defense program to isolate damaged regions in the brain,” increase neuroprotection and start the repair of damaged nervous tissue, including the blood brain barrier, he said. This response, while beneficial, can eventually create more damage if left unchecked. Reactive astrogliosis has a well-documented role in neurological diseases including multiple sclerosis, Alzheimer’s and autism spectrum disorder (the subject of a previous book by Parpura and colleagues). New evidence, detailed in “Astrocytes in Psychiatric Disorders,” suggests that chronic alcohol use can also lead to reactive astrogliosis.
The second major response is astrodegeneration, characterized by thinning and shrinking of astrocytes. This is seen in several neuropsychiatric disorders, including schizophrenia, major depressive disorder, alcohol abuse disorder and obsessive-compulsive disorders. “It all relates to reduce homeostasis of glutamate, and we know that can lead to psychiatric disorders,” Parpura said. Chapters of “Astrocytes in Psychiatric Disorders” highlight emerging research on the critical roles of astrocytes in the “encoding and expression of motivated behaviors relevant to drug addiction” and “the role of astrocytic control of the synaptic efficacy and its dysfunction in the pathophysiology of obsessive-compulsive and related disorders.”
Filling a need
“Astrocytes in Psychiatric Disorders” fills the need for a textbook that can be used in advanced courses/graduate seminars in glial pathophysiology, Parpura says. “It will also be of interest to physicians,” he added. “Psychiatrists are welcoming this idea that astrocytes are involved in these conditions. Clinicians as a rule are most interested in how they can help their patients, no matter what the target is.”
At this stage of research, “we are primarily cataloguing what goes on in these diseases and finding that some of the medicines work through astrocytes, including some antidepressants,” Parpura said. “The next step is to find glial-specific targets for specific diseases, including post-traumatic stress disorder.”