Health & Medicine
May 14, 2025
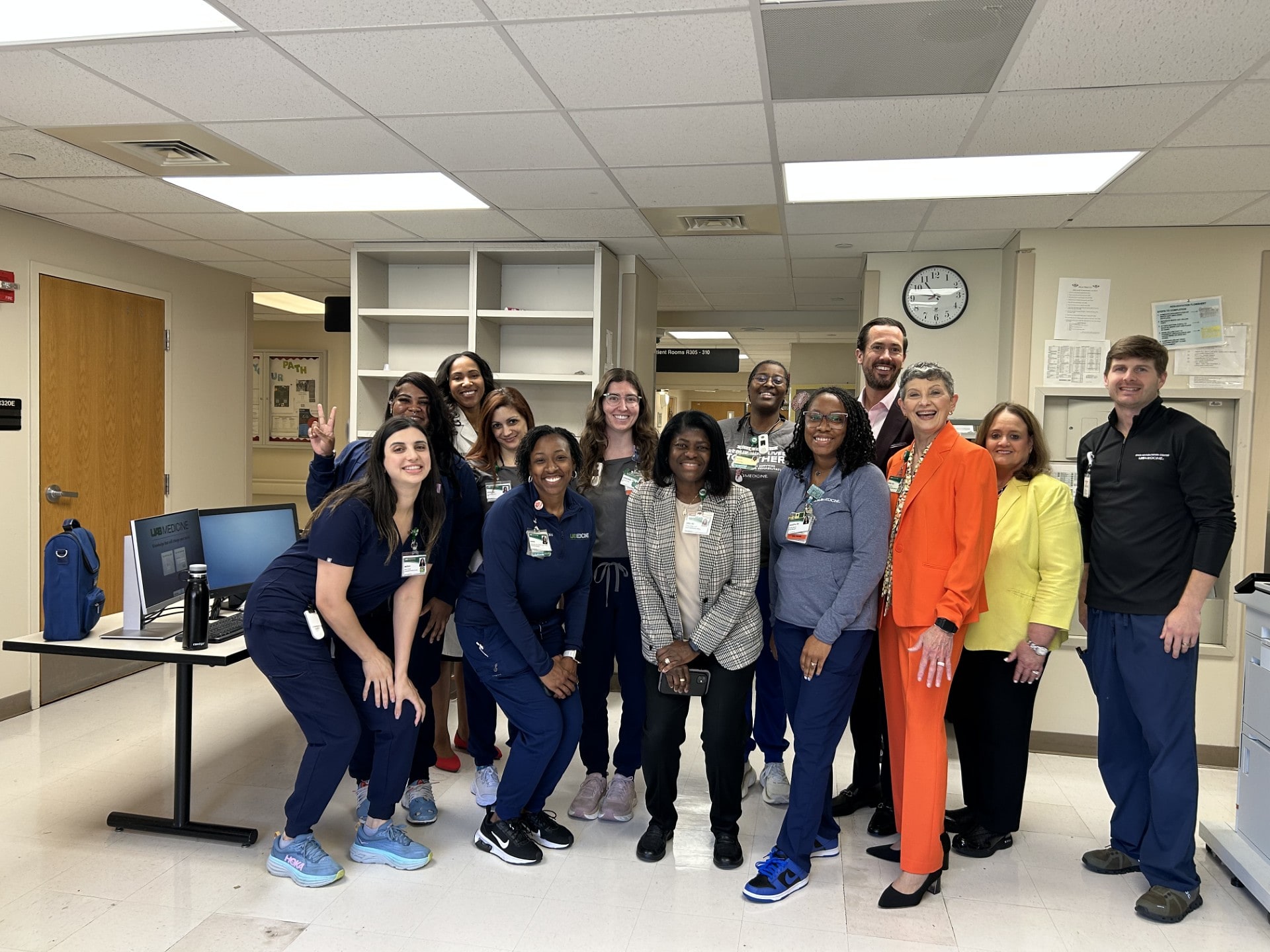
A billboard of gratitude: How one family thanked the nurses who helped welcome their baby girl
Grateful first-time mom thanks labor and delivery nurses in a big way.
Find an Expert
Browse our list of UAB experts who can provide insights on timely news and research. To contact an expert, please coordinate with the public relations specialist associated with each individual.
Find an ExpertCampus & Community
May 12, 2025