Case History
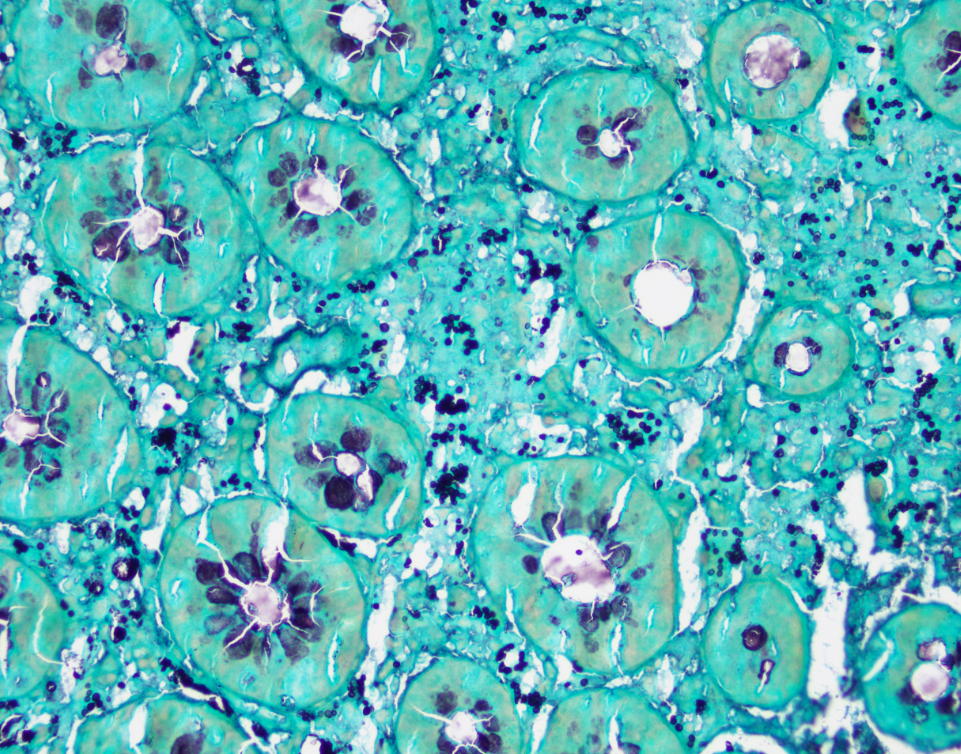
A 30-year-old female with a history of kidney transplantation and immunosuppression presents with chronic diarrhea and fever. A colonoscopy shows mucosal congestion and scattered ulcers. Colon biopsy shows expanded lamina propria with histiocytes. GMS is shown below.
What is the diagnosis?
A. Sarcoidosis
B. Cryptococcus
C. Inflammatory bowel disease
D. Histoplasma
The answer is D. Histoplasma
Discussion:
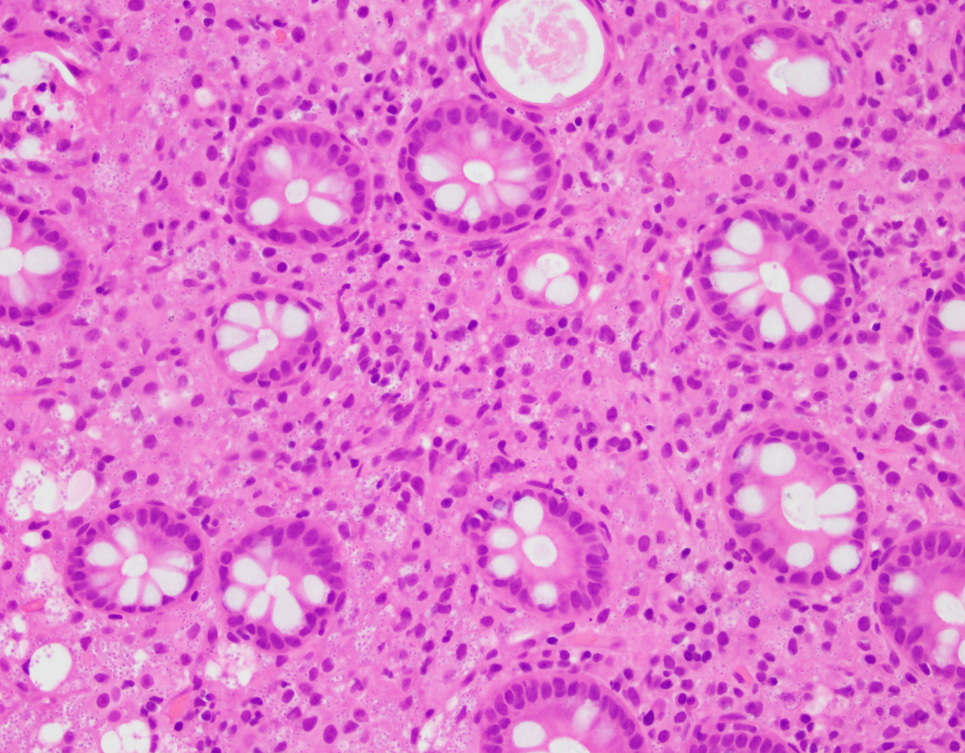
This colon biopsy diagnosis is fungal organisms consistent with Histoplasma species. This patient had positive histoplasma serology and was diagnosed with disseminated histoplasmosis. Antifungals were started and the patient improved.
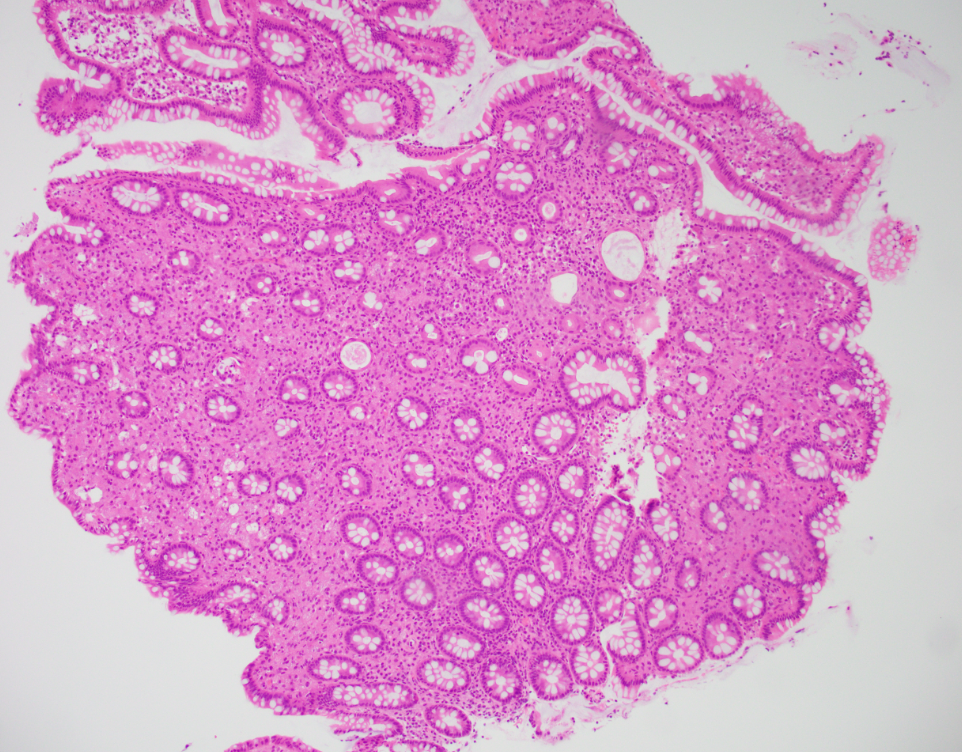
Disseminated histoplasmosis can be seen in immunocompromised patients, and around 80% will have GI involvement. Fever is common and may present as diarrhea, GI bleed, dysphagia, nausea or vomiting. Any part of the GI tract may be involved, with the ileum and colon most commonly. Endoscopy may show ulcers or nodules. Histology shows histiocytic infiltrate in the lamina propria with multiple intracellular organisms that are small and around the same size. The organisms will be GMS positive.
The differential diagnosis for Histoplasma in the GI tract includes other infections, especially other fungal infections. Crytococcus has more variation in organism size and the capsule is mucicarmine positive. Leishmania has a similar appearance on H&E, however is GMS negative. Some other differential diagnoses for histiocytic lesions include sarcoidosis, which usually has well-formed granulomas. Inflammatory bowel disease may have granulomas or ulceration, however no organisms would be seen in histiocytes and GMS stain is negative. Correlation with clinical history, laboratory tests, and endoscopic findings are always helpful.
Case contributed by: Anne Prater, D.O., Surgical Pathology Fellow, UAB Pathology