Case History
The patient was a 31-year-old G1P1 mother, cesarean delivery at 32 weeks. Additional history sought after slide review.
The most likely diagnosis is:
A. Extravillous trophoblasts with benign aytpia
B. Intraplacental choriocarcinoma
C. Lymphoma
D. Metastatic adenocarcinoma
Answer: D. Metastatic adenocarcinoma.
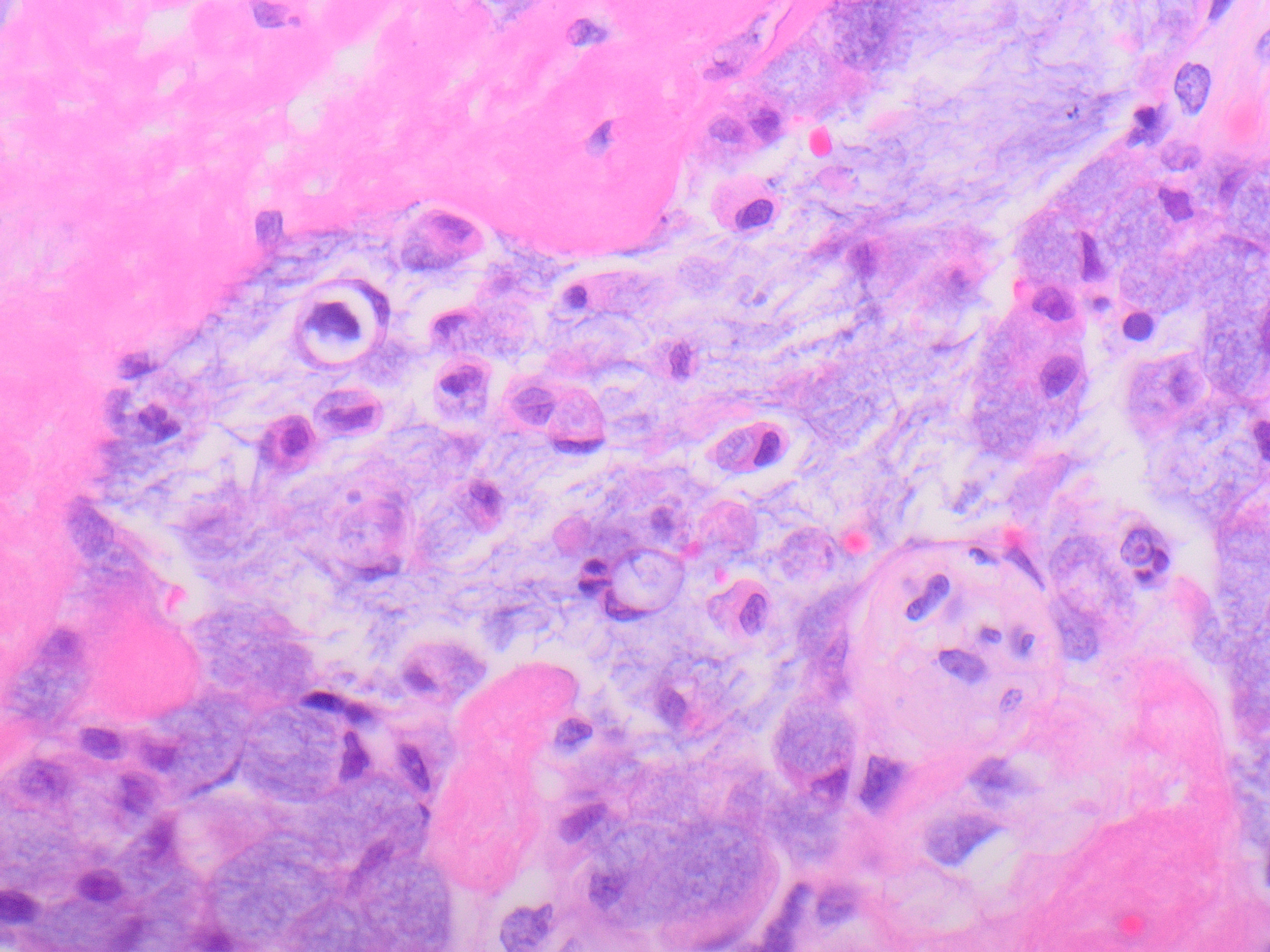
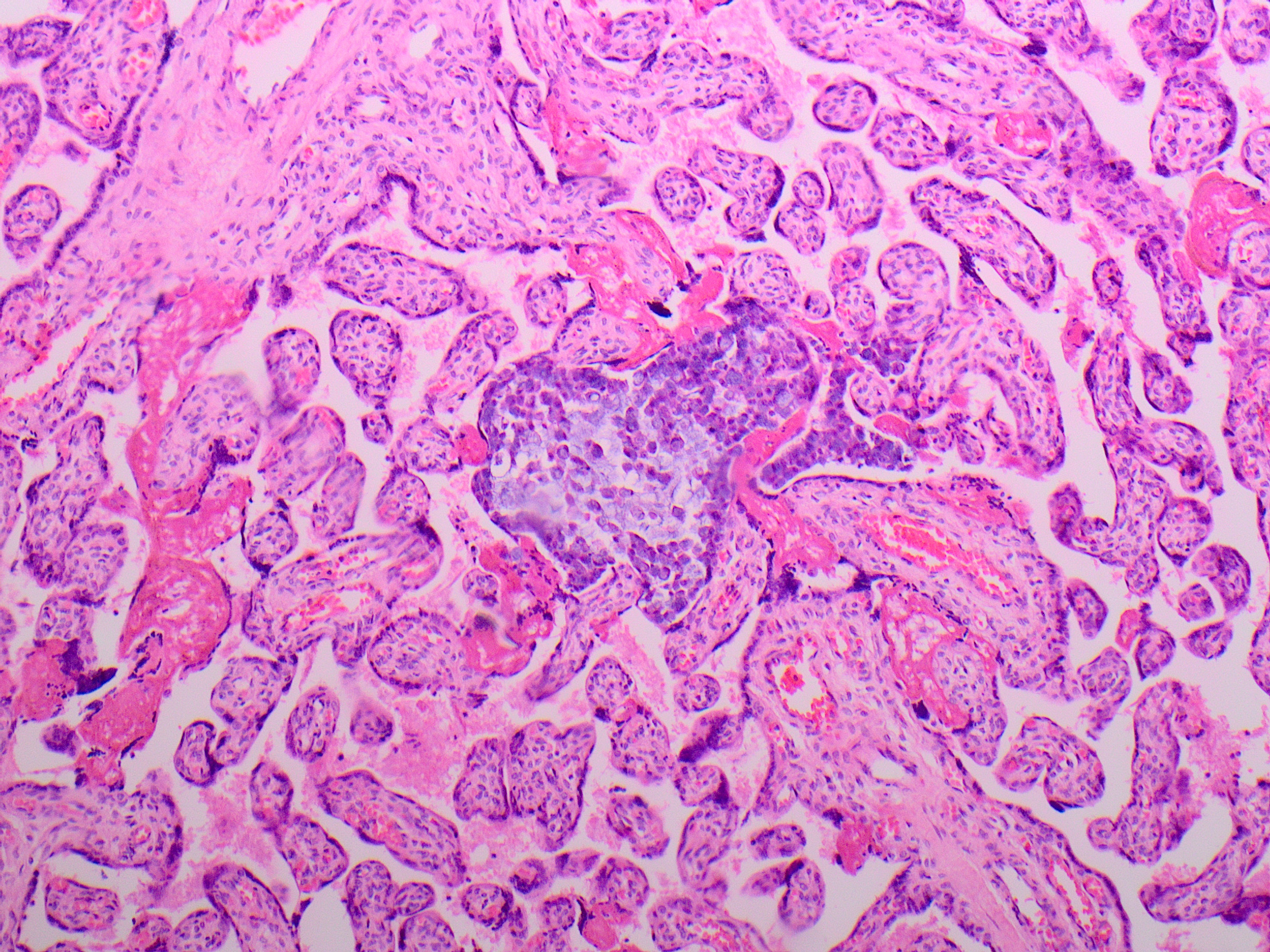
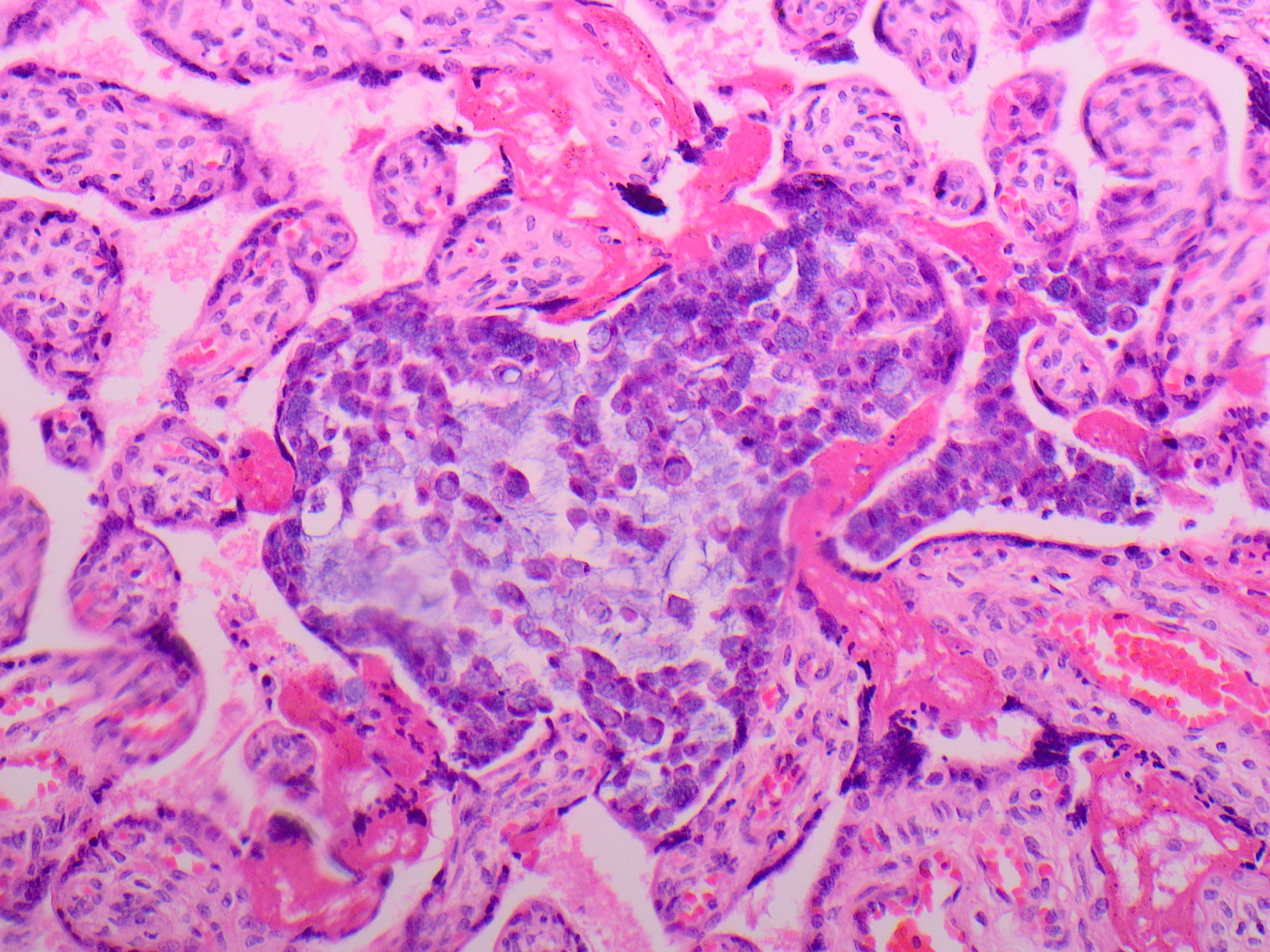
The placenta in this case was low weight for gestation (258g trimmed weight; 290-438g expected), but otherwise grossly unremarkable. Histologically, cohesive clusters of malignant cells were present scattered within the maternal space, with multifocal distribution in all examined sections. Cytologically, the malignant cells were large with high nuclear to cytoplasmic ratio, open nuclear chromatin pattern, and abundant intracellular and extracellular mucin with occasional signet ring cytomorphology. There was no chorionic villous or fetal circulatory involvement. The features are consistent with maternal adenocarcinoma metastatic to the placenta.
Additional maternal history included a known maternal adenocarcinoma of unknown primary, metastatic to the lung. The mother’s malignancy was discovered shortly before delivery, and workup was limited, although an endobronchial biopsy of a lymph node was able to be performed, revealing adenocarcinoma. The cytologic features of the placental metastasis were similar to those of the cells in the endobronchial biopsy material. No intraoperative evidence for abdominal involvement was seen at the time of cesarean delivery. The mother reportedly died during this cesarean section delivery and no autopsy was performed. The baby reportedly did well in the neonatal period.
The cytology and distribution of the malignant cells in the current case are not characteristic of the other answer choices. The cells in the current case are cohesive, and their nuclear features and mucin production distinguish them from lymphoma cells. Occasional small aggregates of markedly atypical extravillous trophoblasts may be seen in otherwise normal placentas, and are of uncertain significance. However, extravillous trophoblasts in that situation are quite large, often multinucleated, with clumped chromatin, and with low nuclear to cytoplasmic ratio and abundant cytoplasm, and do not produce mucin. Choriocarcinoma is a malignancy derived from trophoblasts, with cytologic features similar as described above for trophoblasts, but with marked nuclear atypia which is often extreme. Choriocarcinoma has an intraplacental form that may rarely occur in term placentas, which presents as a mass lesion which may be mistaken for a placental infarction. Choriocarcinoma cells are arranged in a biphasic or triphasic pattern with mononuclear intermediate or cytotrophoblast cells surrounded by multinucleated syncitiotrophoblast cells and often with prominent central necrosis.
Malignancy during pregnancy has an estimated incidence of 1:1000 pregnancies, which has risen in tandem with worldwide trends in delaying childbirth. However, metastasis to the placenta from maternal malignancy is quite rare. There is some evidence that the placenta may present an effective physical barrier, as well as an inhospitable environment due to hormonal and immunologic factors, which together act to decrease tumor growth and spread. Maternal malignancies most commonly reported to metastasize to the placenta include malignant melanoma, breast carcinoma, and
hematologic malignancies. Other solid tumor types are less commonly reported, and include cervical, gastrointestinal of various types, head and neck squamous cell carcinoma, lung, ovarian, and pancreatic.
References:
1. Hui P. Gestational Trophoblastic Tumors: A Timely Review of Diagnostic Pathology. Arch Pathol Lab Med. 2019 Jan;143(1):65-74.
2. Froehlich K, Schmidt A, Heger JI, Al-Kawlani B, Aberl CA, Jeschke U, Loibl S, Markert UR. Breast cancer, placenta and pregnancy. Eur J Cancer. 2019 Jul;115:68-78.
3. Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, Pentheroudakis G; ESMO Guidelines Working Group. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013 Oct;24 Suppl 6:vi160-70.
4. Baergen RN et al. Benirschke’s Pathology of the Human Placenta. Seventh ed. Springer Nature Switzerland. “Other Maternal Disorders Complicating Pregnancy.” Ch. 21, pp. 577-609.