Case History
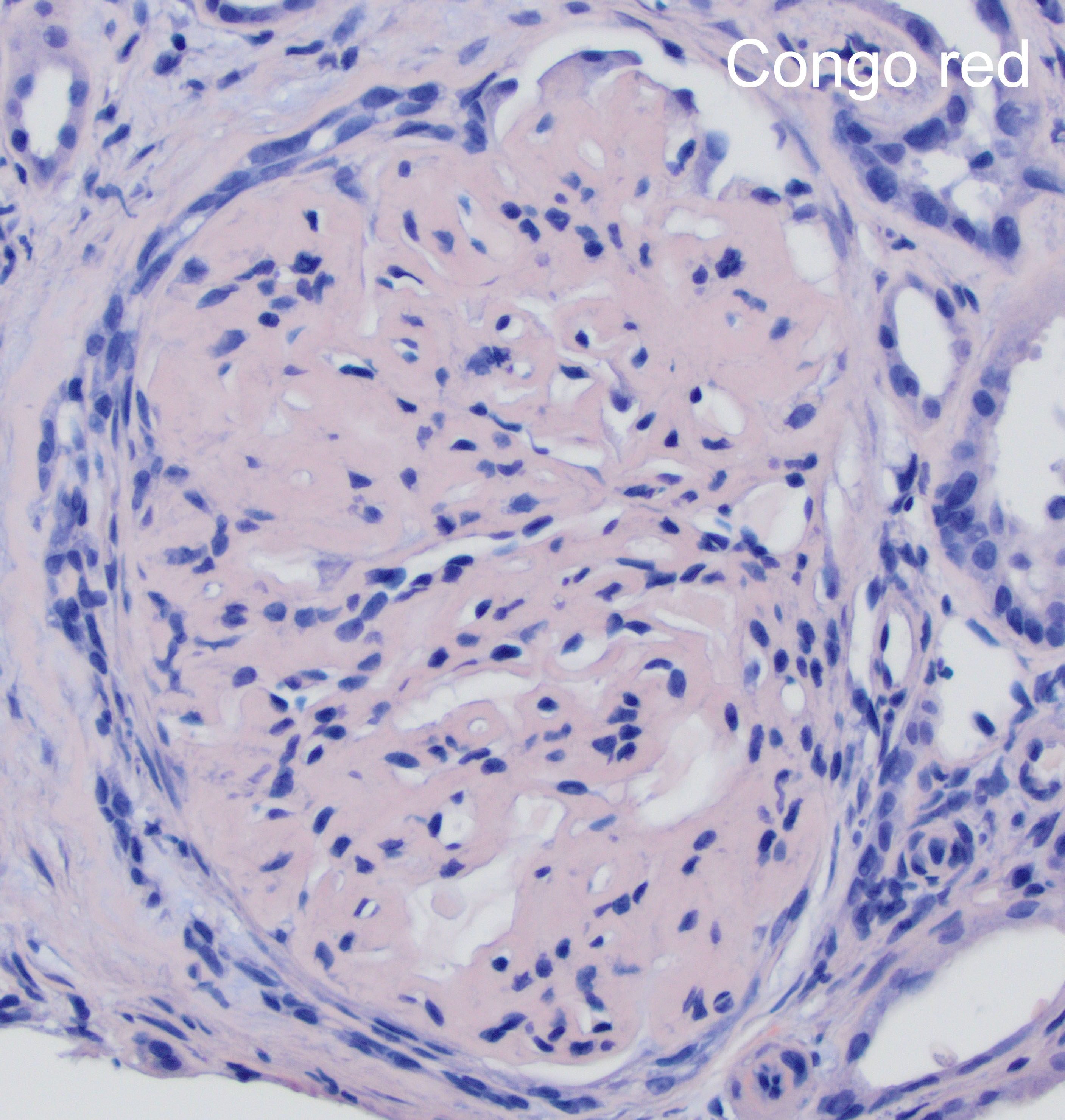
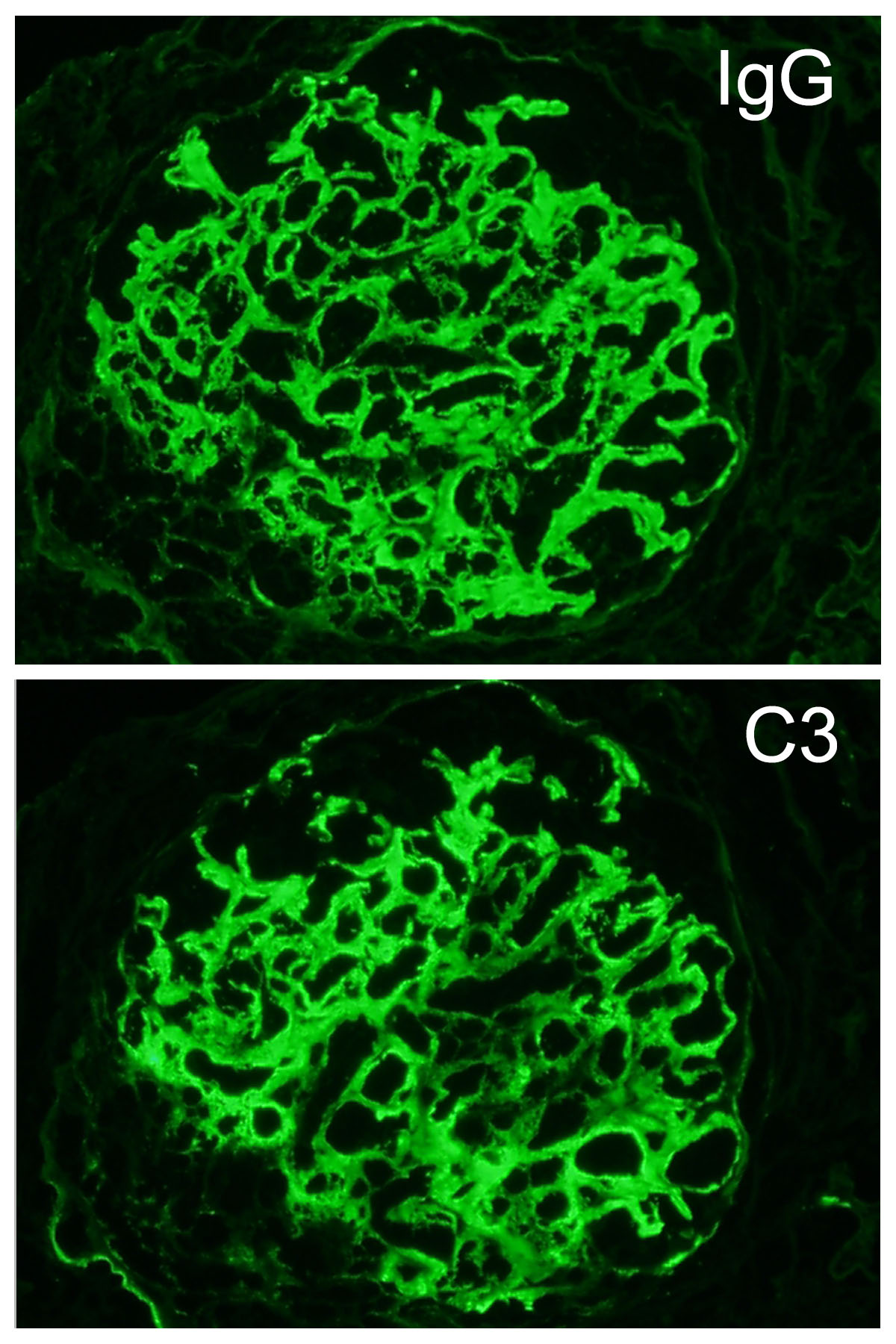
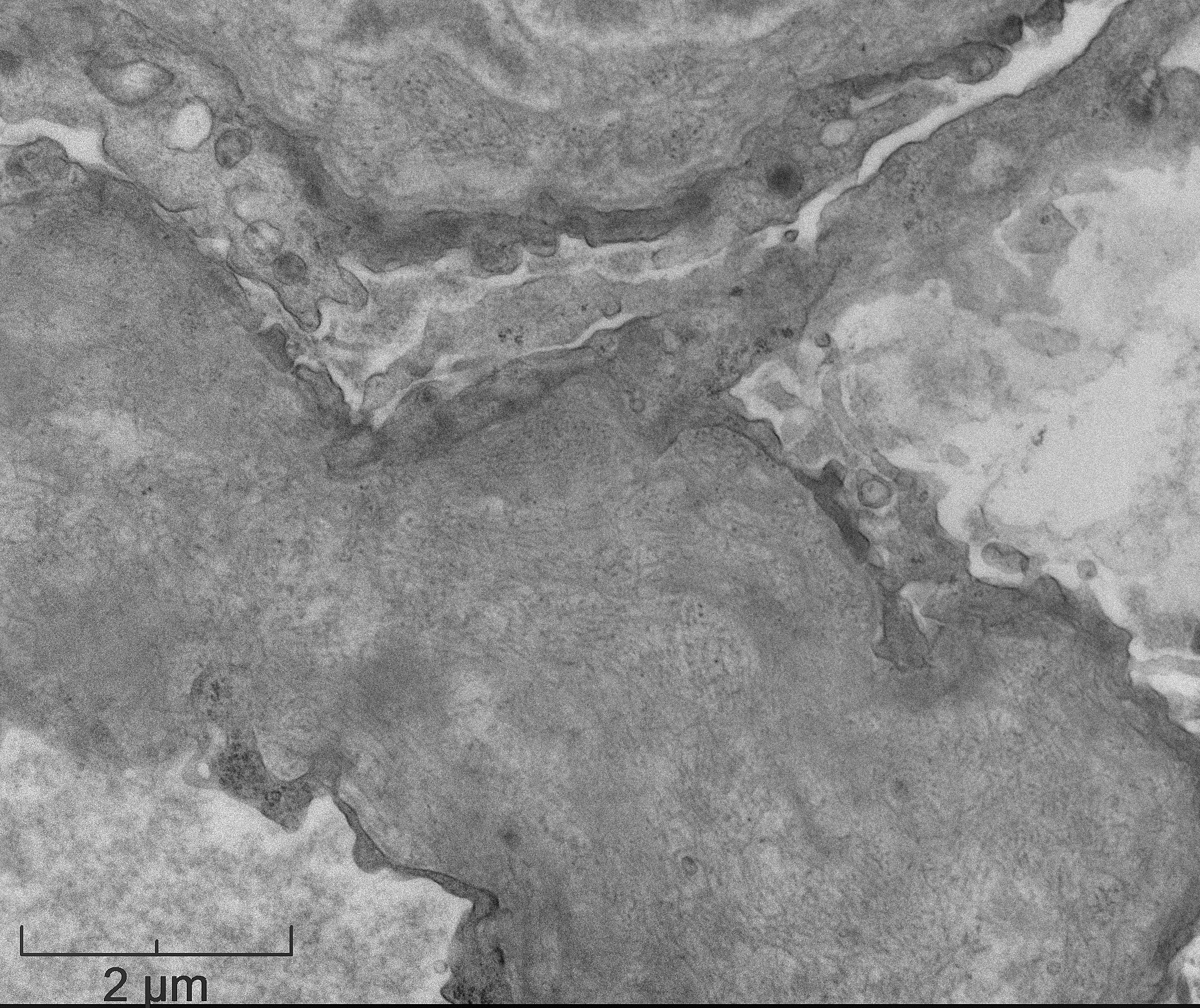
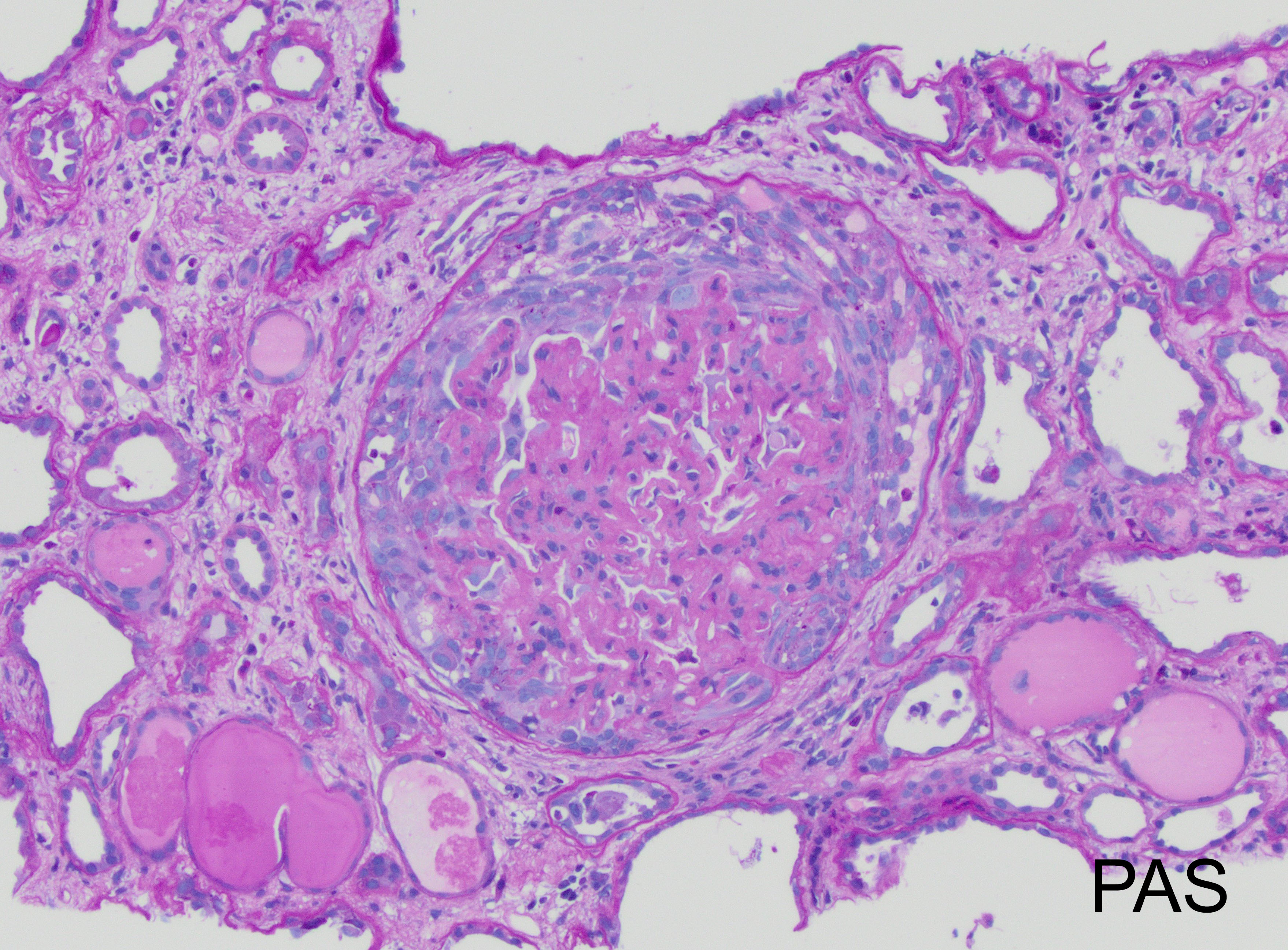
The patient is 32 year-old female with acute kidney injury and nephrotic range proteinuria. A renal biopsy showed diffuse global mesangial and capillary wall expansion by eosinophilic weakly PASH positive material (Silver stain showed in Figure 1), with cellular crescents in 40% and fibrocellular crescents in 5% of the glomeruli. A Congo red stain failed to show apple-green birefringence under polarized light (Figure 2). There was intense immunofluorescence staining with IgG, IgA, C3, and light chains (Figure 3). Electron microscopy showed fibrils with 25 nm average diameter (Figure 4).
What stain would be most helpful to confirm the diagnosis?
- PLA2R
- DNAJB9
- THSD7A
- AA protein

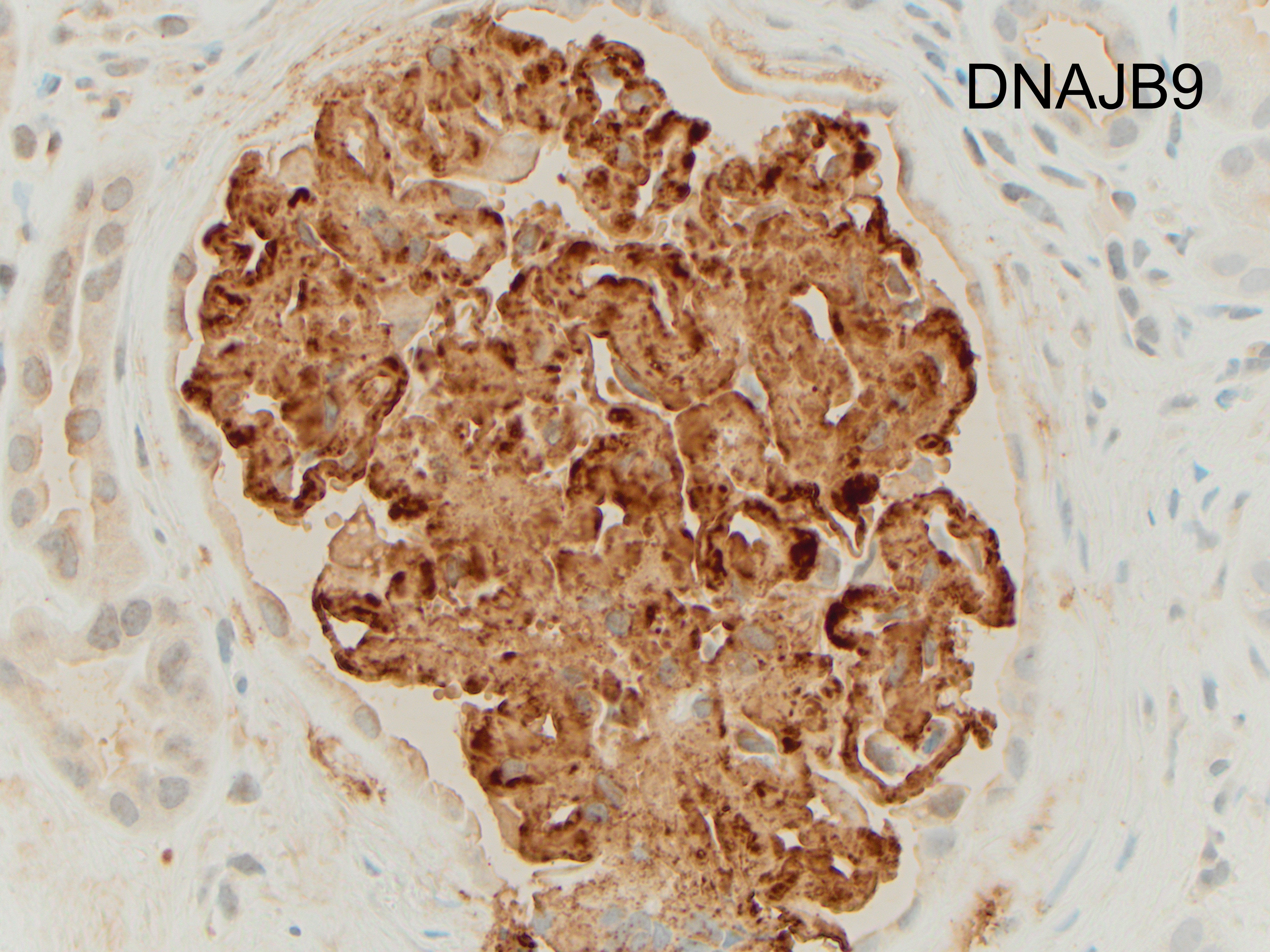
Answer: B: DNAJB9
Discussion:
Immunohistochemical staining for DNAJB9 (DnaJ homolog subfamily B member 9) helps confirm the diagnosis of fibrillary glomerulonephritis (FGN) in this case (Figure). DNAJB9 is a member of the DNA-J heat-shock protein family, that act as co-chaperones for the heat shock protein 70 family members, important chaperones in proper folding, translocation, or degradation of proteins. Although DNAJB9 is expressed at low levels in all cell types, FGN is, at present, the only disease that has been shown to be associated with large amounts of extracellular deposition of this protein.
FGN is a rare form of glomerulonephritis (less than 1% in native renal biopsies), which diagnosis is historically defined by glomerular deposits of Congo red negative, randomly arranged, straight fibrils without a hollow center that measure between 10-30 nm in diameter (larger than amyloid fibrils) and stain for immunoglobulins. The fibrils are localized in the mesangium and/or along the glomerular basement membrane.
Clinically, the patients are usually adults (mean age sixth decade) with a slight female preponderance. An association with autoimmune disease, malignant neoplasms and hepatitis has been reported. At the time of presentation, most have nephrotic range proteinuria, sometimes with nephrotic syndrome, hematuria, and renal insufficiency. Rapidly progressive glomerulonephritis is seen in a minority of the patients. FGN has a poor prognosis with limited treatment options.
By light microscopy, the most commonly reported patterns of injury are membranoproliferative and mesangial proliferative, with focal crescents in 17-50% of the cases (like in this case which showed less than 50% of glomeruli involved; figure). The deposits result in expansion of the mesangium and/or capillary walls by eosinophilic material that is pale with periodic acid-Schiff, nonargyrophilic, and negative for Congo red. By immunofluorescence, “smudgy” mesangial and/or capillary wall intense staining for IgG (most often IgG4 subclass), usually with C3, kappa and lambda light chains is noted. IgM, IgA and C1q show weaker positive staining in some cases.
The distinction between FGN and amyloidosis is made on the basis of Congo red, DNAJB9 (high sensitivity and specificity for FGN) and composition of fibrils by electron microscopy. Immunohistochemistry against AA amyloid may be used to diagnose a specific type of amyloid deposits. PLA2R (M-type phospholipase-A2 receptor) and THSD7A (thrombospondin type-1 domain-containing 7A) are used in the diagnosis of membranous nephropathy.
References:
Nasr SH, Fogo AB. New developments in the diagnosis of fibrillary glomerulonephritis. Kidney International. 2019;96:581–592.
Nasr SH, Vrana JA, Dasari S, et al. DNAJB9 is a specific immunohistochemical marker for fibrillary glomerulonephritis. Kidney Int Rep 2018;3:56-64.
Rosenstock JL, Markowitz GS. Fibrillary glomerulonephritis: An update. Kidney Int Rep 2019;4:917-922.