Case History
A 32-year-old female, with a history significant for tuberous sclerosis, presents with dyspnea. CT imaging demonstrates diffuse bilateral nodular and cystic changes in the lung parenchyma. A wedge lobectomy is received.
Which of the following immunohistochemical stains would best confirm your diagnosis?
Answer choices:
- HMB45, SMA
- SMA, desmin, caldesmon
- STAT6, CD34
- CD117, DOG1
The correct answer is:
A: HMB45, SMA, which would be positive in this case of pulmonary lymphangioleiomyomatosis (LAM), also known as lymphangiomyomatosis.
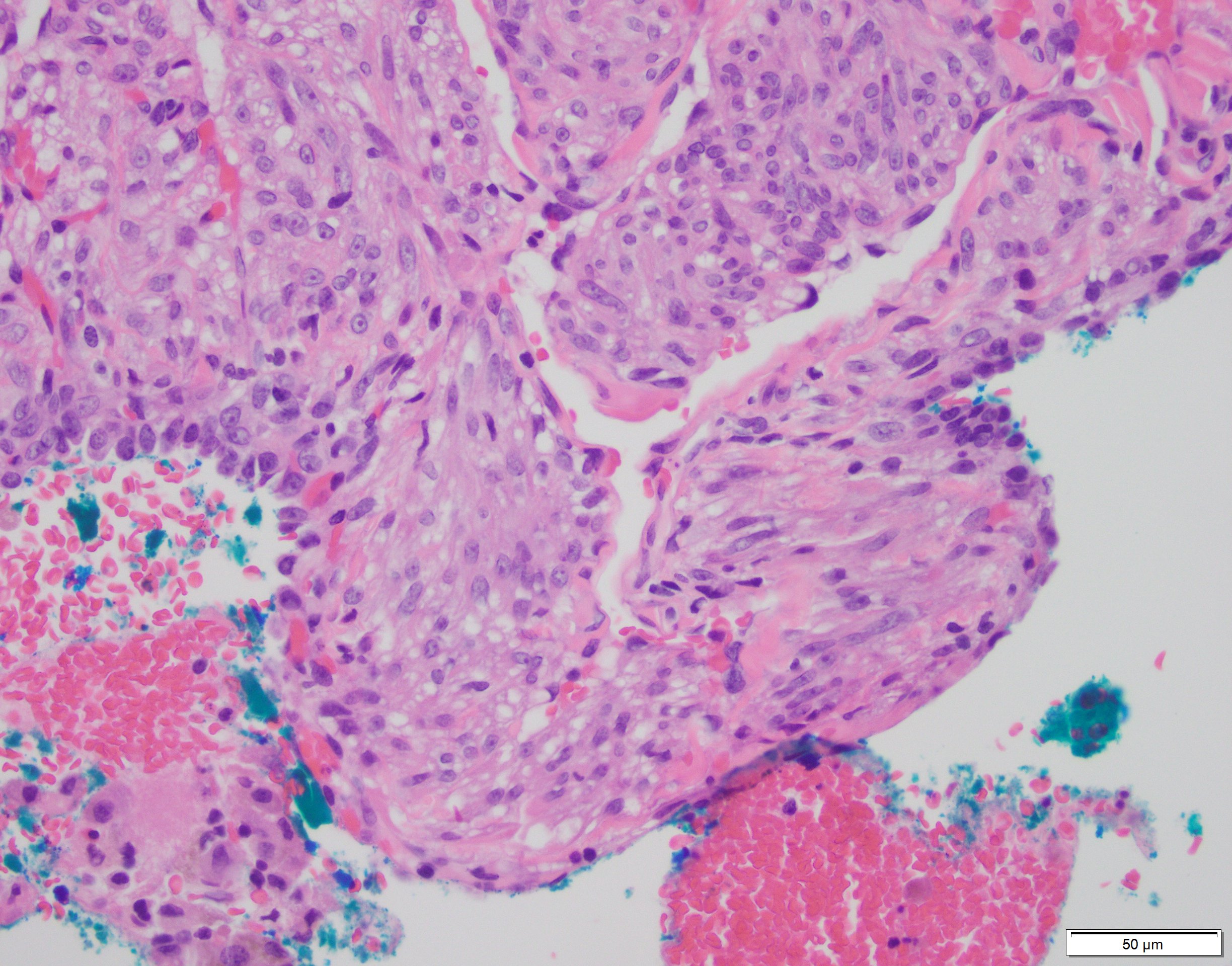
LAM is a rare non-neoplastic interstitial lung disease, almost exclusively seen in premenopausal women and has a disease association with tuberous sclerosis in a subset. The tumor is characterized by a bland spindled or epithelioid proliferation, belonging to the so-called PEComa family of tumors, named aptly for Perivascular Epithelioid Cell differentiation. The PEComa family of related mesenchymal neoplasms include angiomyolipoma, lymphangiomyomatosis, and clear cell "sugar" tumor of the lung. As a family, these tumors characteristically share immunoreactivity for melanocytic (HMB45 or melanA) and smooth muscle markers (SMA and/or desmin)[1].
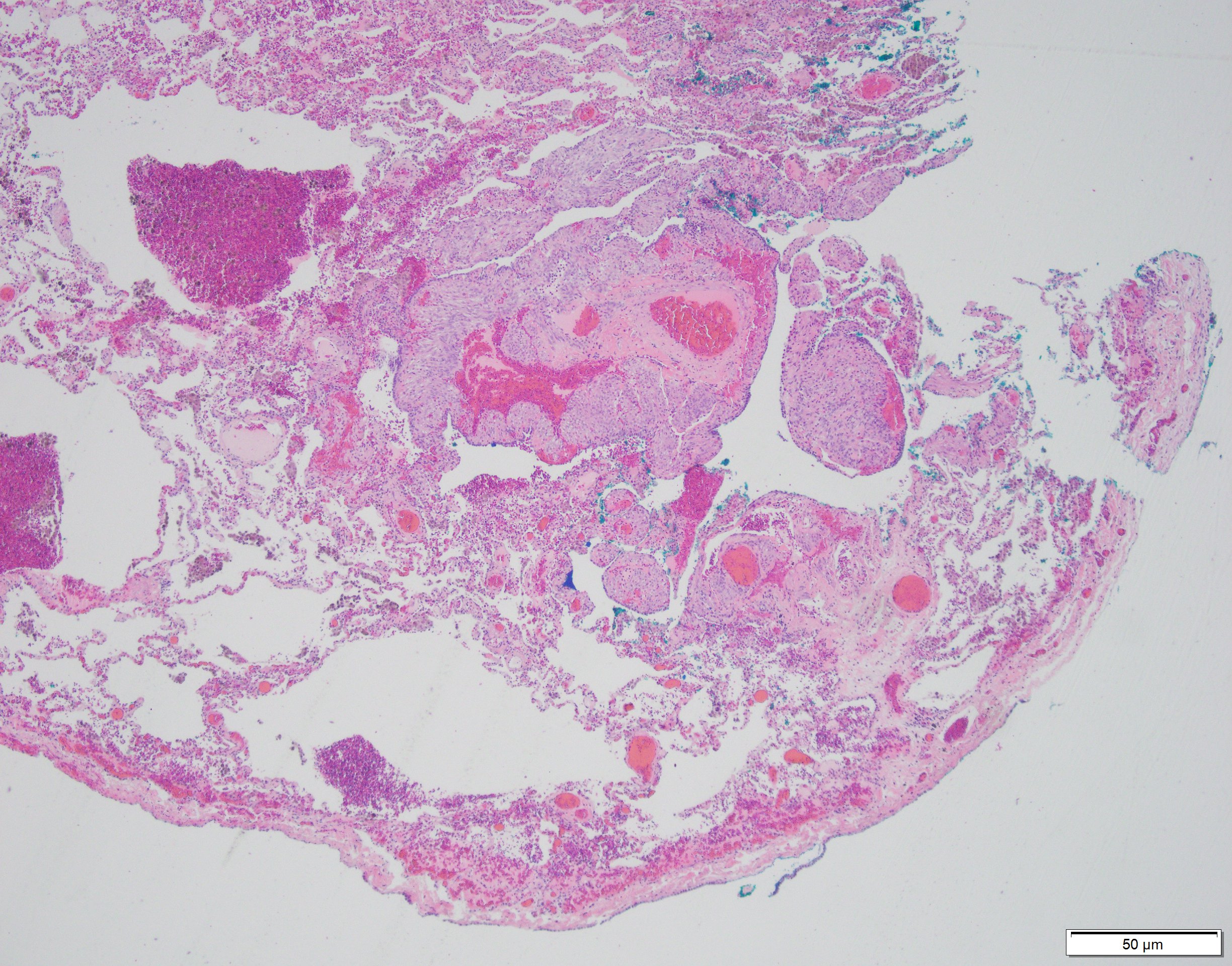
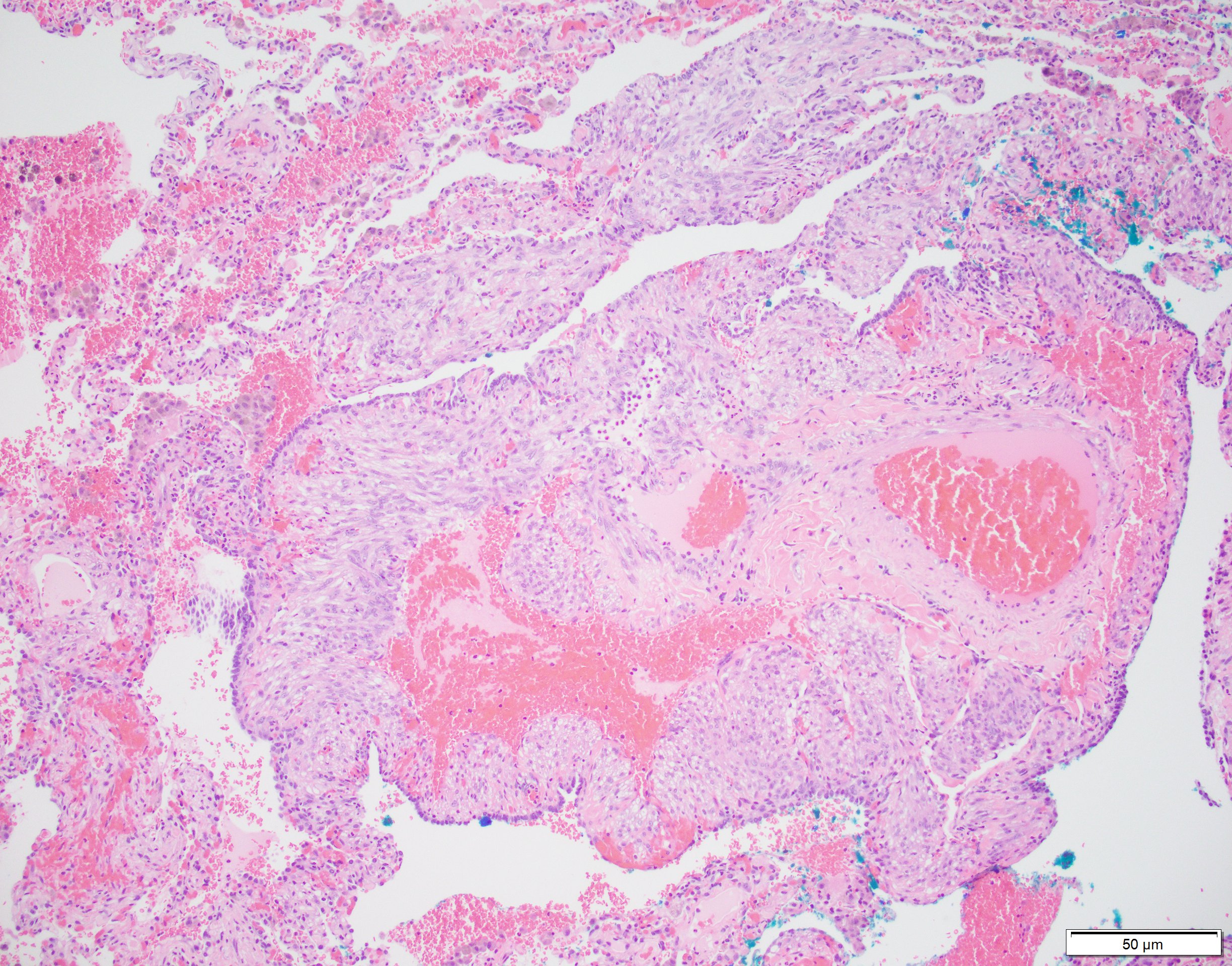
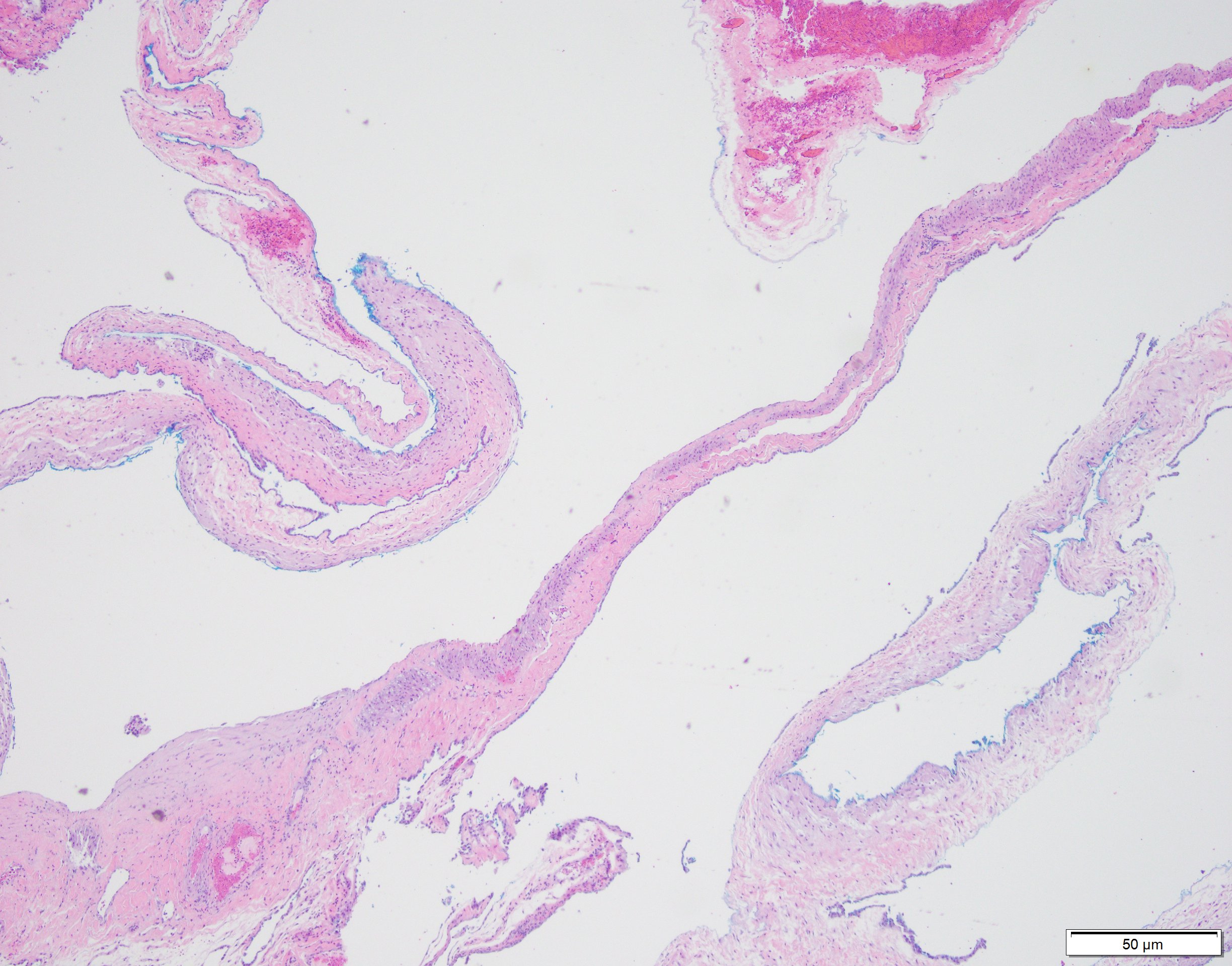
Low power view shows cysts lined by a thickened wall and random areas of expanded interstitium. Higher power shows these expanded areas occupied by bland, short, plump, myoid spindly cells, with eosinophilic or cleared cytoplasm. The so-called “LAM” cells are positive for HMB45, and also SMA, ER, and PR [2].
Extrapulmonary cases of LAM have been described occurring in mediastinal lymph nodes and uterus sites. Thus, a differential diagnosis includes leiomyoma, which the later usually forms a discreet nodular mass, and would lack in classic cystic spaces. LAM can be distinguished from a leiomyosarcoma (e.g. metastacizing low grade leiomyosarcoma) by the lack of significant mitoses and pleomorphism.
Another underrecognized harmartomatous proliferation that can occur in Tuberous Sclerosis complex-associated LAM is micronodular pneumocyte hyperplasia, which are cellular nodules of hyperplastic alveolar pneumocyte proliferations accompanied by numerous intra-alveolar macrophages, that can be mistaken for adenocarcinoma-in-situ without the classic knowledge of the clinical history [2]. High-resolution Computed Tomography may be diagnostic for LAM, demonstrating characteristic cysts, so a biopsy may not be needed. Prognosis for patients with LAM is linked to complications of cyst rupture and pneumothorax, such as when subpleural-located cysts rupture [3].
References:
J L Hornick and C D M Fletcher. PEComa: what do we know so far? Histopathology. 2006; 48; 75–82.
Anna-Luise A. Katzenstein. Diagnostic Atlas of Non-Neoplastic Lung Disease. Springer Publishing Company. 2016; 44-50.
Abbott Gerald F, et al. Lymphangioleiomyomatosis: Radiologic-Pathologic Correlation. RadioGraphics. 2005; 25:803– 828.
Case contributed by: Marsha Xiong, M.D., UAB Pathology, GI Pathology Fellow