Schick awarded MAOA grant
 Department of Orthopaedic Surgery Research Fellow Samuel Schick was awarded the Mid-America Orthopaedic Association Education Grant for Senior Residents/Fellows to attend the 2023 Annual Meeting.
Department of Orthopaedic Surgery Research Fellow Samuel Schick was awarded the Mid-America Orthopaedic Association Education Grant for Senior Residents/Fellows to attend the 2023 Annual Meeting.
The Mid-America Orthopaedic Association is the regional orthopedic society for orthopedic surgeons within the 20 central U.S. states. This organization strives to serve its members through educational and fellowship opportunities, as well as providing value-added services throughout the year.
Schick’s award totals $2,500 and allows him to attend the 40th Mid-America Orthopaedic Association Annual Meeting in Miramar Beach, Florida. This annual meeting allows orthopaedic faculty to engage and explore subspecialty education through instructional courses, symposia, ask-the-expert sessions, breakout sessions, and posters.
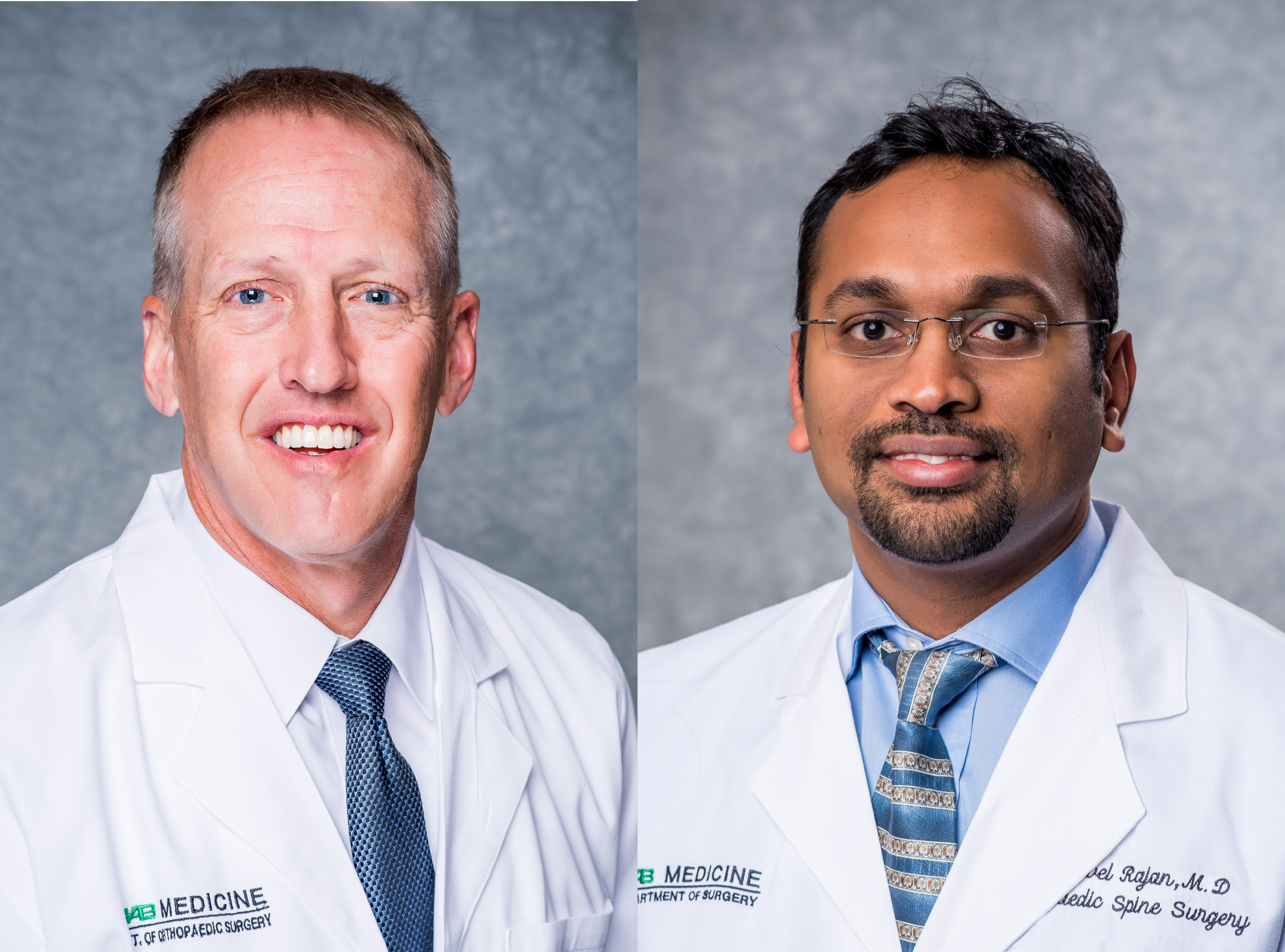
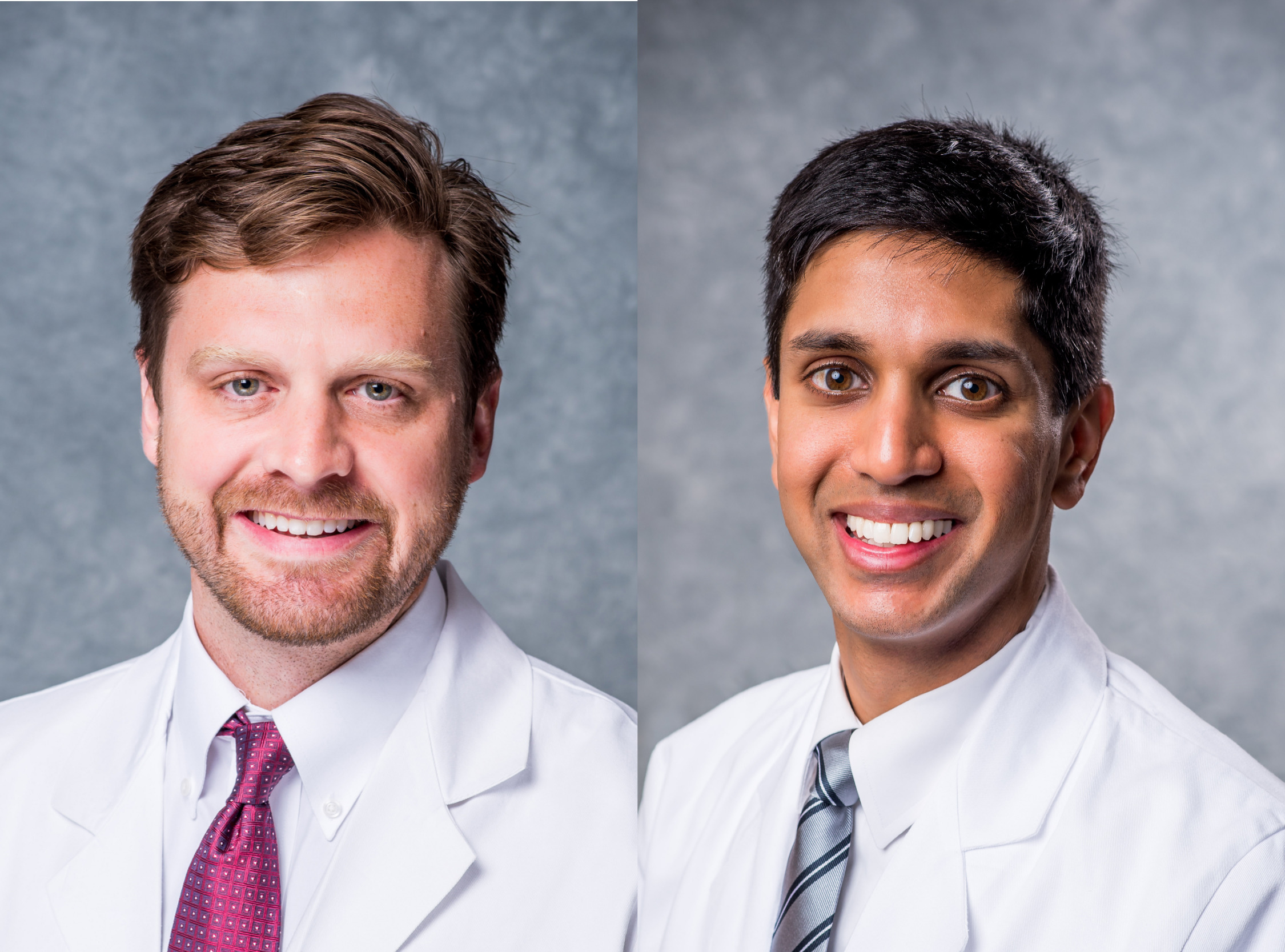
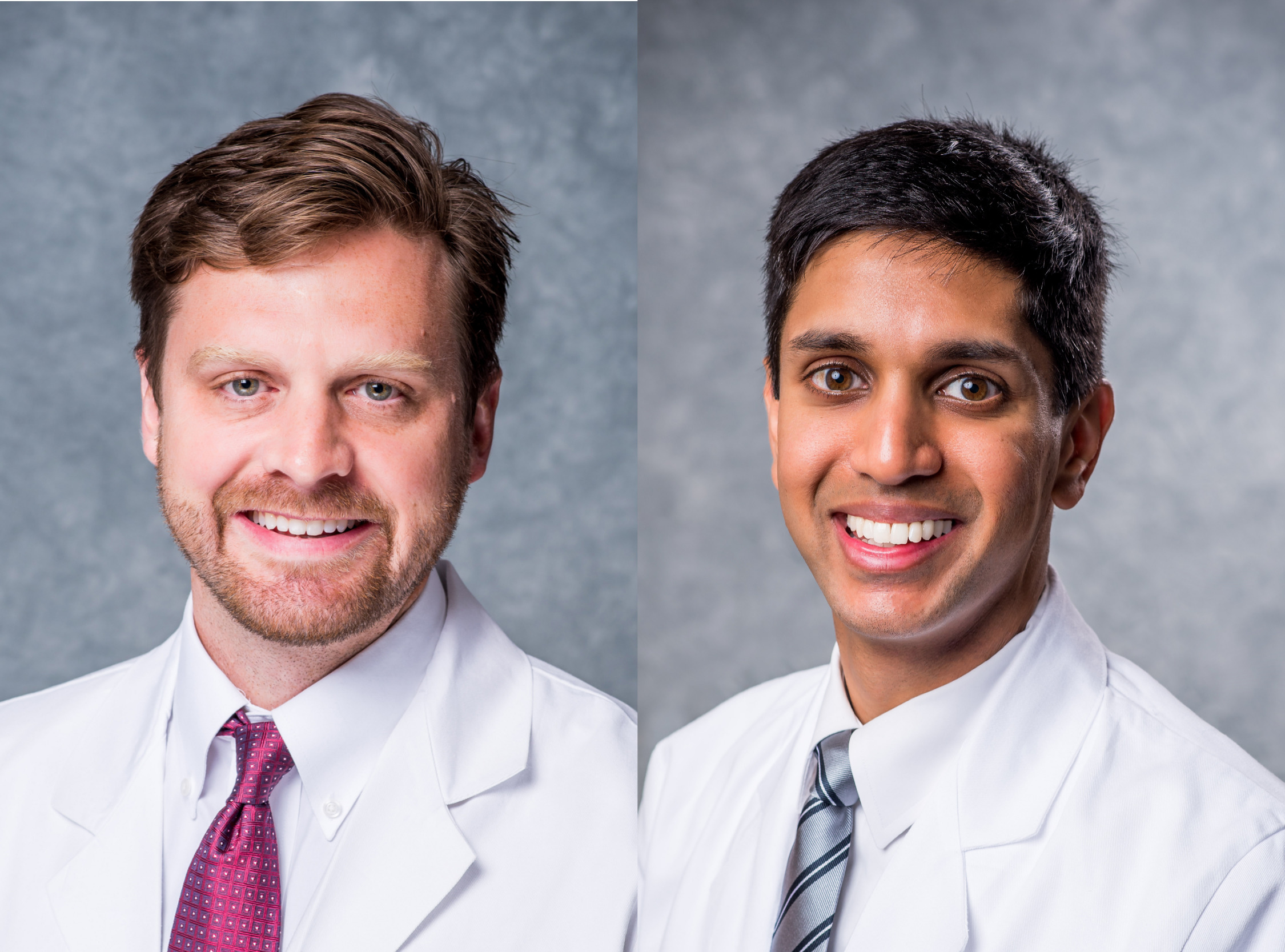
Department welcomes Hiatt & Morsy
 The Department of Orthopaedic Surgery is pleased to welcome Luke Hiatt, M.D., and Mohamed Morsy, M.D., as assistant professors of orthopaedic surgery. Hiatt joins the spine service, while Morsy joins the hand and upper extremity service.
The Department of Orthopaedic Surgery is pleased to welcome Luke Hiatt, M.D., and Mohamed Morsy, M.D., as assistant professors of orthopaedic surgery. Hiatt joins the spine service, while Morsy joins the hand and upper extremity service.
Hiatt received his medical degree from the University of Texas Houston Health Science Center, during which time he was elected to the Alpha Omega Alpha honor society. He completed his residency at the University of Alabama at Birmingham, where he developed an interest for treatments of spinal conditions and deformities and elected to pursue subspecialized training in spine surgery.
Before joining the department in 2023, Hiatt completed his fellowship in orthopaedic spine surgery at the University of California, Davis near Sacramento, CA. There, he further researched degenerative spine conditions, as well as complex techniques for treatment of severe spinal deformities.
Morsy received his medical degree from Assiut University in Egypt. He also completed his residency at Assiut University in Egypt, where he was inducted as a member of the Egyptian Orthopaedic Association, AO Trauma Foundation and SICOT-International Society of Orthopaedic Surgery and Traumatology.
Before joining the department in 2023, Morsy completed his fellowship in microsurgery and peripheral nerve surgery at Assiut University in Egypt, as well as completed his research fellowship in the Division of Plastic Surgery at the Mayo Graduate School of Medicine in Rochester, MN. There, he further researched the reconstruction of elbow and hand functions, hand fractures, vascular grafts and arterial perforator flaps.
The Return - Fitzgerald Mofor
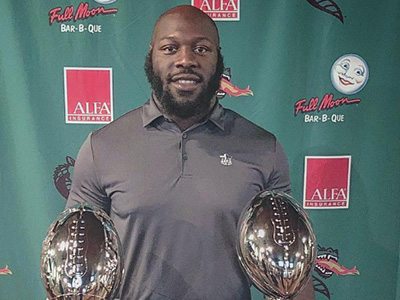 The UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
The UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
Theiss named co-chair of international comprehensive spine course
 UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., has been named co-chair of the joint North American Spine Society and Arab Spine Society comprehensive spine course. Additionally, Dr. Theiss will be co-chair of the upcoming Dubai International Spine Conference in May.
UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., has been named co-chair of the joint North American Spine Society and Arab Spine Society comprehensive spine course. Additionally, Dr. Theiss will be co-chair of the upcoming Dubai International Spine Conference in May.
The comprehensive spine course is set for May 14-16, 2023 in Dubai, United Arab Emirates. This course is designed for neurosurgeons, orthopedists, spine specialists and spine related physicians to acquire advanced knowledge on the evaluation of spinal disorders, spinal disease process and surgical skills. This event gives health care professionals involved in the spinal treatment spectrum an opportunity to get best practices in the specialty of spine.
The 22nd Dubai International Spine Conference will follow the course on May 17-19, 2023. This conference presents the latest surgical techniques, research and management strategies to current and future spine specialists. The overall goal is to share state-of-the-art technology and techniques to clinicians in an effort to improve patient outcomes.
Momaya selected to AANA Education Committee
 The Arthroscopy Association of North America has selected UAB Department of Orthopaedic Surgery Associate Professor Amit Momaya, M.D., as a member of their Educational Committee.
The Arthroscopy Association of North America has selected UAB Department of Orthopaedic Surgery Associate Professor Amit Momaya, M.D., as a member of their Educational Committee.
The AANA is an international, non-profit organization of more than 5,000 orthopaedic surgeons who are committed to advancing the field of minimally invasive orthopaedic surgery to improve patient outcomes. The AANA Education Committee provides coordination and oversight of the high-quality continuing medical education (CME) activities the organization provides.
Momaya will serve as a member of the education committee for two years, from 2023 to 2025. His term will officially begin at the 2023 AANA Annual Meeting on May 6, 2023, in New Orleans, Louisiana.
Your guide to UAB Ortho at AAOS 2023
 UAB Department of Orthopaedic Surgery faculty and trainees will head to the American Academy of Orthopaedic Surgeons 2023 Annual Meeting in Las Vegas, Nevada from March 7-11.
UAB Department of Orthopaedic Surgery faculty and trainees will head to the American Academy of Orthopaedic Surgeons 2023 Annual Meeting in Las Vegas, Nevada from March 7-11.
Spine Team publishes study on postoperative Ileus risk factors
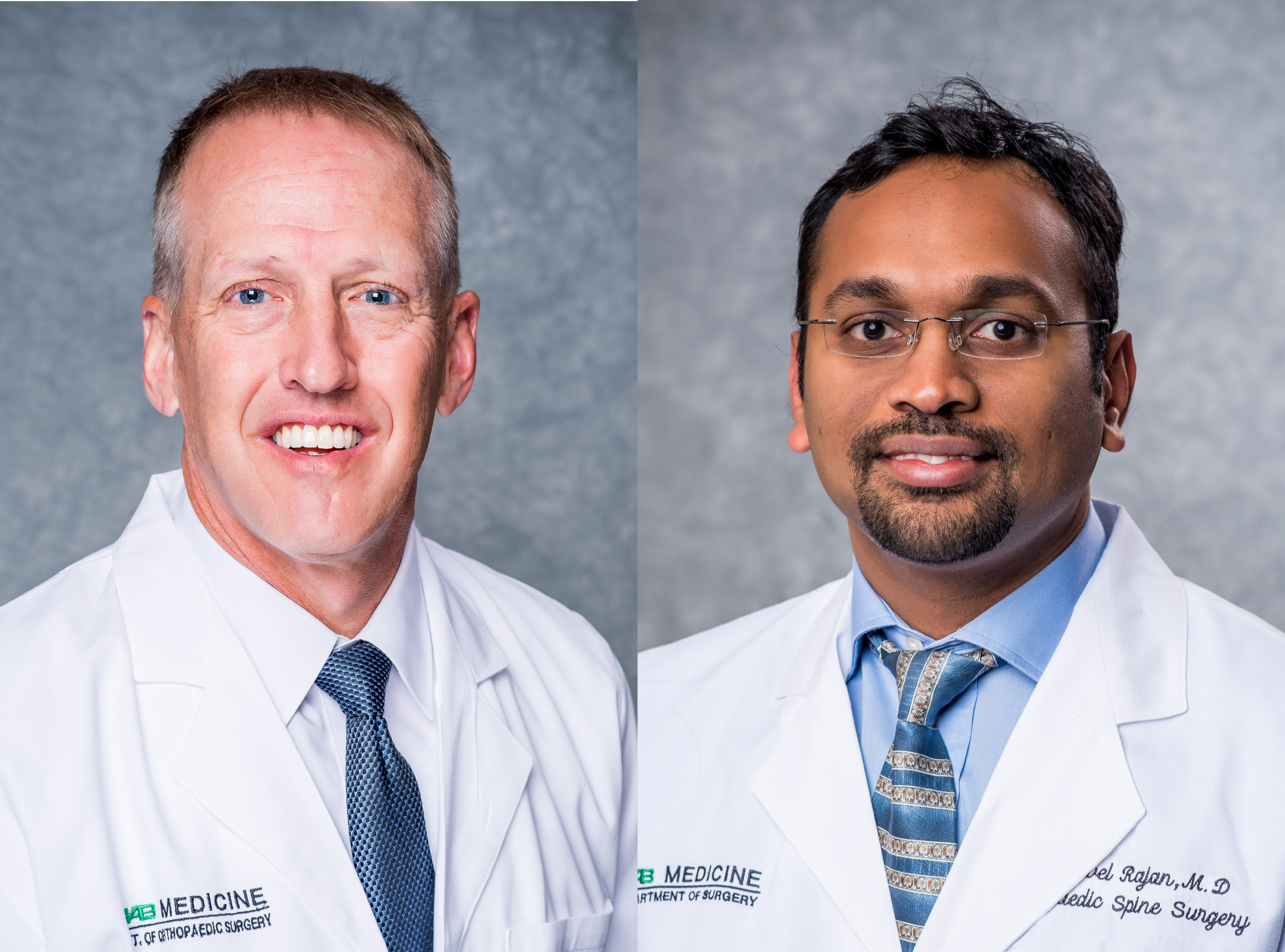
 UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., alongside Associate Professor Sakthivel Rajaram Manoharan, M.D. and former Research Fellow Logan Reed, published a study addressing the risk factors of postoperative ileus after spinal fusion surgery.
UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., alongside Associate Professor Sakthivel Rajaram Manoharan, M.D. and former Research Fellow Logan Reed, published a study addressing the risk factors of postoperative ileus after spinal fusion surgery.
This study was published in October of 2022 in the World Neurosurgery Journal and is titled “Risk Factors for Postoperative Ileus After Thoracolumbar and Lumbar Spinal Fusion Surgery: Systematic Review and Meta-Analysis.”
Postoperative ileus is a common complication, a generalized impairment of gastrointestinal motility found after spine surgery. This specific complication has a reported incident range of 10 to 30 percent among most surgical patients.
The study group conducted a comprehensive search of ten articles compromising a total of 297,809 patients showing ileus symptoms after the surgical treatment of spinal pathologies. Variables including gender, age, body mass index, comorbidities, approach, type of surgery performed, levels fused, anesthesia time and length of stay were considered as the main outcomes of measurement.
Results of the study showed that postoperative ileus after lumbar surgery had a statistically significant association with increased age, surgical time, anesthesia time, estimated blood loss, and length of stay. Furthermore, individuals who underwent spinal fusion had higher odds of postoperative ileus if they were male, if an anterior approach was performed or if less than three vertebral levels were fused. Body mass index did not show any association with postoperative ileus.
The study concludes that risk factors associated with postoperative ileus after spinal fusion surgery include male gender, older age, longer surgical times, higher estimated blood loss, longer lengths of stay, greater numbers of levels of fusion and anterior surgical approach.
You can read more on this study and its results here.
Department presents research at NASS & OTA Conferences in late 2022

UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., former Associate Professor Elie Ghanem, M.D., and former Research Fellow Logan Reed displayed their research study entitled "Utility of next-generation sequencing and isothermal microcalorimetry for identification of bacteria in presumed aseptic thoracolumbar revision spine surgery" at the NASS Conference. Reed presented this study, which determined the rate of bacterial presence in revision thoracolumbar spinal instrumentation surgery due to an implant failure.
 Associate Professor Clay Spitler, M.D., Associate Professor Jon Quade, M.D., Orthopaedic Surgery Resident David Patch, M.D., and former Research Fellow Logan Reed presented their research study entitled "Bone Marrow Aspirate with Allograft Cancellous Chips Versus Autologous ICBG or RIA in the Treatment of Long Bone Nonunions" at the OTA Conference. Patch presented this study, which assessed union rates between bone marrow aspirate with allograft cancellous chips (BMA-ACC) compared to autologous iliac crest bone grafting (ICBG) and the reamerirrigator-aspirator (RIA) system in the treatment of long bone nonunion.
Associate Professor Clay Spitler, M.D., Associate Professor Jon Quade, M.D., Orthopaedic Surgery Resident David Patch, M.D., and former Research Fellow Logan Reed presented their research study entitled "Bone Marrow Aspirate with Allograft Cancellous Chips Versus Autologous ICBG or RIA in the Treatment of Long Bone Nonunions" at the OTA Conference. Patch presented this study, which assessed union rates between bone marrow aspirate with allograft cancellous chips (BMA-ACC) compared to autologous iliac crest bone grafting (ICBG) and the reamerirrigator-aspirator (RIA) system in the treatment of long bone nonunion.
Associate Professor Clay Spitler, M.D., also presented at the OTA Conference with his own work entitled "The use of Computed Tomography Angiography to predict Complications in Tibia Fractures". This study assessed the ability of CTA findings to predict complications in limbs that do not require vascular surgical intervention.
The North American Spine Society (NASS) Conference was held in October 2022 in Chicago, Illinois. The Orthopaedic Trauma Association (OTA) Conference was also held in October 2022 in Tampa, Florida.
Mabry on UAB MedCast
 The Department of Orthopaedic Surgery Assistant Professor Scott Mabry, M.D., was a recent guest on UAB Medicine's podcast - UAB MedCast. This podcast series is geared toward medical professionals who wish to learn about new advances in academic medicine and surgery. This on-the-go tool allows listeners to collect continuing medical education credit with each episode.
The Department of Orthopaedic Surgery Assistant Professor Scott Mabry, M.D., was a recent guest on UAB Medicine's podcast - UAB MedCast. This podcast series is geared toward medical professionals who wish to learn about new advances in academic medicine and surgery. This on-the-go tool allows listeners to collect continuing medical education credit with each episode.
Mabry’s episode entitled “Outpatient Total Joint Replacement: The Future is Now”, discusses many advances in anesthesiology, pain management and physical therapy, making total joint replacement a popular outpatient surgery. These interdisciplinary improvements have made same-day total joint replacement preferable for many patients.
He further discusses the importance of proper patient selection, the kind of team that successfully coordinates this outpatient procedure, and how your patients might benefit.
Subscribe to UAB MedCast and listen to Dr. Mabry’s episode anywhere you listen to podcasts. Or listen on their webpage here.
Siegel to be Surgeon Faculty for Complex Hip & Knee Revision Symposium
 UAB Department of Orthopaedic Surgery Professor Herrick Siegel, M.D. has been selected to be on the Surgeon Faculty for the Johnson & Johnson Institute - Complex Hip & Knee Revision Symposium.
UAB Department of Orthopaedic Surgery Professor Herrick Siegel, M.D. has been selected to be on the Surgeon Faculty for the Johnson & Johnson Institute - Complex Hip & Knee Revision Symposium.
The event will be held in Phoenix, AZ on Saturday, January 28, 2023.
The Complex Hip Revision Symposium is designed to be an interactive hands-on learning experience on innovative MedTech solutions for the treatment of revision hip procedures as well as periprosthetic femur fractures.
The faculty panel includes both trauma-trained and joint reconstruction-trained surgeons to offer their unique perspectives on the treatment of revision hip procedures, periprosthetic fractures, and distal femur replacement procedures. The expert faculty panel will walk participants through case presentations and discuss the treatment algorithms they use for their patients.
Symposium details can be viewed by clicking here.
Boohaker receives Frontline Champion Award
 UAB Department of Orthopaedic Surgery Andrea Boohaker, CRNP was named "Frontline Champion” for the Opioid Stewardship Program during UAB Quality Week 2022.
UAB Department of Orthopaedic Surgery Andrea Boohaker, CRNP was named "Frontline Champion” for the Opioid Stewardship Program during UAB Quality Week 2022.
The Opioid Stewardship Program at UAB Medicine supports and advocates for patient-centered, effective, and safe pain management and opioid prescribing practices. The Opioid Stewardship Committee is an interdisciplinary team with representation from across UAB Medicine.
"I was very humbled and proud to represent both Ortho and Neurosurgery and to participate in this initiative,” says Boohaker.
To see the full list of UAB Quality Week 2022 Award winners, click here.
Brabston and Momaya publish study on orthopedic consequences of modern gladiators
 UAB Department of Orthopaedic Surgery Associate Professor Will Brabston, M.D., alongside Associate Professor Amit Momaya, M.D., and former Research Fellow Joseph Elphingstone, M.D., published a study addressing the lower extremity musculoskeletal issues found with National Football League (NFL) athletes.
UAB Department of Orthopaedic Surgery Associate Professor Will Brabston, M.D., alongside Associate Professor Amit Momaya, M.D., and former Research Fellow Joseph Elphingstone, M.D., published a study addressing the lower extremity musculoskeletal issues found with National Football League (NFL) athletes.
The study was published in September of 2022 in The Physician and Sportsmedicine Journal, titled “Orthopedic consequences of modern gladiators: a systematic review of lower extremity musculoskeletal issues in retired NFL players.”
Lower extremity musculoskeletal issues are very common among athletes of contact sports. These issues can be classified as bone fractures, joint dislocation, direct blows to any muscles, sprains, etc. The most common side effects of these issues are sharp pain, aching, stiffness and burning sensations in the affected area. Current literature shows the short-term effects of these injuries rather than long-term outcomes of playing professional football.
The study accessed nine cohort studies evaluating lower extremity arthritis in retired NFL athletes, as well as data from individual studies, including demographic information (age, body mass index, length of career, position), injury descriptions (location of injury, number of injuries, diagnoses), and procedure (total knee and or hip arthroplasty) frequency.
Results of the study showed arthritis in retired NFL players was more than twice as prevalent than in the general United States male population at 95 percent. Ankle osteoarthritis was directly correlated with the number of foot and ankle injuries they sustained while playing. Players who are 50 years of age and older had a 16.1 and 13.8 times higher risk of undergoing total knee arthroplasty and total hip arthroplasty, respectively, when compared to the general population. In older age groups, this trend held with retired NFL players being at least 4.3 and 4.6 times more likely than members of the general population to undergo these procedures, respectively.
The study demonstrates that the effects of NFL-related lower extremity injuries extend beyond the players’ careers and present a higher risk for early-onset osteoarthritis and overall frequency of undergoing total knee and hip arthroplasty.
You can read more about this study and its results here.
Spine Team publishes study on Unilateral atlanto-occipital injury
 UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., alongside Associate Professor Sakthivel Rajaram Manoharan, M.D., former Research Fellow Logan Reed, and former Spine Fellow Jacob Lepard, M.D., published a study addressing the likeliness of safe, non-operative treatment methods for a unilateral atlanto-occipital injury.
UAB Department of Orthopaedic Surgery Professor and John D. Sherrill Chair of Orthopaedic Surgery Steven Theiss, M.D., alongside Associate Professor Sakthivel Rajaram Manoharan, M.D., former Research Fellow Logan Reed, and former Spine Fellow Jacob Lepard, M.D., published a study addressing the likeliness of safe, non-operative treatment methods for a unilateral atlanto-occipital injury.
This study was published in September in the Journal of Craniovertebral Junction & Spine (JCJS) and is titled “Unilateral atlanto-occipital injury: A case series and detailed radiographic description”.
An atlanto-occipital injury is a rare and unstable injury of the craniocervical junction, associated with high-energy trauma caused by the hyperextension of the skull, found in car accidents and intense fall victims.
The study evaluated eight patients with a mean age of 45 years old. All eight patients experienced some form of neurological trauma. Causes of this trauma included motor vehicle collision for five patients (5/8, 62.5%), falls for two patients (2/8, 25%), and assault for one patient (1/8, 12.5%). All patients had a widened condyle-C1 interval >2 mm. Three patients underwent occipitocervical fusion, one patient underwent atlantoaxial fusion, and another received subaxial fusions for other injuries. Three patients underwent no surgical intervention. All of these patients were seen at least once as an outpatient following hospital discharge. There were no delayed neurologic injuries or deaths after the performance of this study.
The study concludes that a ligament injury at the craniocervical joint functions more as a spectrum rather than a dichotomous diagnosis, which a subset of this can likely, be safely managed non-operatively.
To read more about the study and its results, click here.
Siegel accepted into Surgical Leadership Program at Harvard
 UAB Department of Orthopaedic Surgery Professor Dr. Herrick Siegel has been accepted to the Surgical Leadership Program at Harvard Medical School.
UAB Department of Orthopaedic Surgery Professor Dr. Herrick Siegel has been accepted to the Surgical Leadership Program at Harvard Medical School.
This leadership program offers in-depth training for surgeons seeking to acquire the nontechnical, executive skills needed to step into leadership positions and excel as heads of departments, divisions, projects and institutions. This program comprises a term of one year, beginning in March 2023 and concluding in March 2024.
Siegel has a rich history of surgical excellence and treats all facets of orthopedic joints, including both oncology and arthritic disorders. His specific clinical interests include limb salvage procedures in pediatric and adult patients; as well as management of bone loss secondary to metastatic disease, primary bone malignancy and revision total joint surgery.
Johnson selected to Future Trauma Leaders Program
 UAB Department of Orthopaedic Surgery Assistant Professor Dr. Joseph Johnson has been elected to the American College of Surgeons Committee on Trauma (COT) Future Trauma Leaders (FTL) program.
UAB Department of Orthopaedic Surgery Assistant Professor Dr. Joseph Johnson has been elected to the American College of Surgeons Committee on Trauma (COT) Future Trauma Leaders (FTL) program.
The FTL program offers in-depth training and mentoring opportunities to junior trauma and acute care surgeons. Membership comprises a term of two years, beginning with the Committee’s Annual Meeting in March 2023 and concluding with the Clinical Congress meeting in October 2024.
Dr. Johnson treats all facets of orthopedic trauma, including both acute and chronic pathology. His specific clinical interests include pelvic and acetabular fractures, nonunions, and malunions and peri-articular fracture care.
The Return – Keagan McEwan
 Each day, the UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
Each day, the UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
Brabston and Momaya publishes study on Allograft reconstruction for HS and RHS lesions
 UAB Department of Orthopaedic Surgery Associate Professor Will Brabston, M.D., alongside Associate Professor Amit Momaya, M.D., published a study addressing the outcomes of allograft reconstruction on osseous humeral head defects such as Hill-Sachs (HS) or Reverse Hill-Sachs (RHS) lesions.
UAB Department of Orthopaedic Surgery Associate Professor Will Brabston, M.D., alongside Associate Professor Amit Momaya, M.D., published a study addressing the outcomes of allograft reconstruction on osseous humeral head defects such as Hill-Sachs (HS) or Reverse Hill-Sachs (RHS) lesions.
The study was published this month in the Journal of Shoulder and Elbow Surgery (JSES) and is titled “Allograft reconstruction for humeral head defects in the setting of shoulder instability: a systematic review.”
Hill-Sachs (HS) or Reverse Hill-Sachs (RHS) lesions are impaction-type defects in the head of the humerus bone, often associated with recurrent shoulder dislocations. There are many surgical techniques that address these types of injuries but no study has reviewed the outcomes of allograft reconstruction in HS or RHS lesions in a systematic manner.
The team of researchers at UAB reviewed 84 allograft-treated patients, 44 with HS legions and 40 with RHS legions. The average age of HS legion patients was 27 years and RHS legion patients were 43 years of age. Patients with HS legions had a greater postoperative range of motion and average Constant-Murley score (87.9) than those with RHS legions (80.1). In addition, 20.5% of HS patients experienced postoperative complications, whereas 42.5% of RHS patients had postoperative complications.
The study concludes that osteochondral allograft reconstruction for large HS and RHS lesions is acceptable albeit with some complication risk. Patients with HS legions experienced significantly fewer complications than those with RHS lesions after surgery.
To read more about the study and its results, click here.
The Return - Lynley Jackson
 Each day, the UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
Each day, the UAB Sports and Exercise Medicine program supports the community and provides care to patients from across the Southeast. Each story is unique and shows the determination and grit our patients possess. We are honored to be a part of their care team and are happy to share their stories. We hope it provides some inspiration to others on their journey to their Return.
Back in 2021, avid runner and Oak Mountain High School band member, Lynley Jackson, faced a difficult time. Her mother, Kristin, shares her story:
 My daughter, Lynley, started to have some significant pain in her knee in 2021 that was limiting her activity. We were worried because she is a very active person. We visited with Dr. Momaya, who recognized immediately that she had an osteochondral lesion in the knee. He recommended surgery to help address it. He was patient and explained in great detail all of our options. We decided to proceed with surgery.
My daughter, Lynley, started to have some significant pain in her knee in 2021 that was limiting her activity. We were worried because she is a very active person. We visited with Dr. Momaya, who recognized immediately that she had an osteochondral lesion in the knee. He recommended surgery to help address it. He was patient and explained in great detail all of our options. We decided to proceed with surgery.
The surgery was done minimally invasive with just poke holes in the knee. He drilled holes behind the lesion to help with blood flow and also fixed the osteochondral lesion with two screws that will dissolve over time. Her postoperative care was smooth and well planned out. He provided us with a specific physical therapy regimen to follow.
She has done great and is now about one year out and fully healed and back to her usual activities. She no longer has pain when running. She also participates in marching band. We are grateful for the care by Dr. Momaya and his staff!
A Brief History of UAB's Orthopaedic Legacy
 Dr. John D. Sherrill (right) meets with the Monday Morning Quarterback Club, 1944.Authors: David A. Patch, MD, Matthew C. Hess, MD, Michael D. Johnson, MD, Steven M. Theiss, MD
Dr. John D. Sherrill (right) meets with the Monday Morning Quarterback Club, 1944.Authors: David A. Patch, MD, Matthew C. Hess, MD, Michael D. Johnson, MD, Steven M. Theiss, MD
Not surprisingly, in a region where football and an appetite for charity have supported many initiatives, the history of the UAB Department of Orthopaedic Surgery and the orthopaedic surgery residency program has also benefitted from these forces. The story of the Department of Orthopaedic Surgery at the University of Alabama at Birmingham (UAB) and “The Hospital Football Built” are inseparable. This, combined with the vision and leadership of Dr. John Doke Sherrill, paved the way for generations of orthopaedic excellence.
Dr. John D. Sherrill was born in Hartselle, Alabama in 1892. After finishing the two-year curriculum at the Birmingham Medical College in 1915 (BMC’s last class), he practiced briefly with his father in Hartselle, AL before entering WWI. After the war, Dr. Sherrill returned to Birmingham where he pioneered the specialty of orthopaedic surgery, his passion.
His commitment to selfless ideals would lead to his appointment as the first UAB Chief of Orthopaedic Surgery. Dr. Sherrill also served as the first orthopaedist for the University of Alabama’s football team before becoming the Surgical Director of the Crippled Children’s Clinic and Hospital (1934-1968) where he rendered care to children during the poliomyelitis “polio” epidemic. Dr. Sherrill was instrumental in helping to build the Cripple Children’s Hospital in the UAB Medical Center for young polio patients along with the help of donations from organizations including the Monday Morning Quarterback Club and from citizens in the community.
The onset of the United States polio epidemic began between the late 19th-early 20th century, triggering widespread fear of its paralytic potential across the country. In Birmingham, one of the most enduring relief efforts began with a small group of driven individuals at 630 North 19th Street, who opened the first Crippled Children’s Clinic there. However, the clinic quickly became overwhelmed with hundreds of applications for affected children. In response, a fundraising campaign referred to as the “365 Club” requiring only $3.65 a year (one cent a day) stepped up to help. While these efforts were paramount in sustainability, the need for services for affected children continued to grow and in 1936 the clinic was relocated to 11th Avenue and 25th Street North which for the first time offered 40 beds with multidisciplinary services, including operating rooms, a swimming pool, x-ray equipment, hydrotherapy, and several iron lungs. As the epidemic unfolded, it became apparent that the game of football offered hope for the children of Alabama and their families. In the early 1930s, Dr. Sherrill helped originate a series of high school football games launched at Legion Field to benefit the Crippled Children’s Clinic. Those early benefit games transformed into larger contests between freshman teams from universities including Birmingham-Southern College, Samford, and Auburn to support the Children’s Clinic.
However, as the polio pandemic grew and surrounding counties relied on the clinic for support, needs quickly exceeded the capacity of the clinic- at one point 9,000 children with polio in Alabama were on the waitlist to be seen. Meanwhile, a sports editor of The Birmingham News, Henry Hardin “Zipp” Newman, had a vision of combining his love of football with supporting the fight against polio. In 1939, he would go on to establish the “Monday Morning Quarterback Club” to unite local football fans and help provide funding for the Crippled Children’s Clinic. What started as a gathering for fellowship among football lovers quickly grew into one of the most generous civic clubs in the country, drawing support from legendary college football coaches. Club members were instrumental in establishing the foundation of Alabama’s Children’s Hospital.
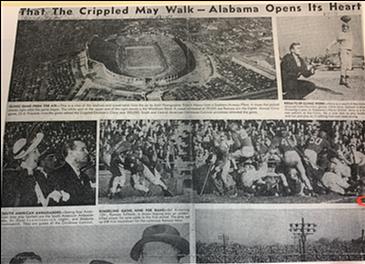 Annual Crippled Children’s Clinic football game. In 1941 the club sponsored and organized the first Crippled Children’s Clinic Game. This game was an annual high school football game that raised money for the Crippled Children’s Hospital to render care for children struck with polio. Later on, in 1943, the event was moved to Thanksgiving Day and specifically reserved for a high school championship game at Legion Field, featuring the top two teams in Birmingham. Polio patients themselves would often come to cheer on the high school athletes in the championship game. It became evident that the determination demonstrated on the gridiron was making a difference in the lives of young polio patients. By 1951 a new $3 million 100-bed Crippled Children’s Clinic and Hospital was opened at 620 South 19th Street. Its unique “wedding cake” appearance enabled children to sunbathe on the patios and included a state of-the-art polio ward. On Thanksgiving Day of 1951, a monument placed outside of the building was dedicated to the Quarterback Club and read “The Hospital Football Built."
Annual Crippled Children’s Clinic football game. In 1941 the club sponsored and organized the first Crippled Children’s Clinic Game. This game was an annual high school football game that raised money for the Crippled Children’s Hospital to render care for children struck with polio. Later on, in 1943, the event was moved to Thanksgiving Day and specifically reserved for a high school championship game at Legion Field, featuring the top two teams in Birmingham. Polio patients themselves would often come to cheer on the high school athletes in the championship game. It became evident that the determination demonstrated on the gridiron was making a difference in the lives of young polio patients. By 1951 a new $3 million 100-bed Crippled Children’s Clinic and Hospital was opened at 620 South 19th Street. Its unique “wedding cake” appearance enabled children to sunbathe on the patios and included a state of-the-art polio ward. On Thanksgiving Day of 1951, a monument placed outside of the building was dedicated to the Quarterback Club and read “The Hospital Football Built."
 Crippled Children’s Clinic and Hospital. Under the leadership of Dr. Sherrill, the Crippled Children’s Hospital served the Birmingham community for over 20 years helping polio patients transition back into their daily lives. Once the disease was largely eradicated in late 1960’s the hospital became repurposed and in 1969 became part of the University of Alabama at Birmingham. The Crippled Children’s Foundation was later formed which continues its mission in fighting childhood diseases today. Though the original “Hospital Football Built” has since been torn down and UAB’s Spain-Wallace Building now stands in its place, the spirit of its presence remains. Since that time, over $29 million has been contributed by the club and the Crippled Children’s Foundation to charitable organizations.
Crippled Children’s Clinic and Hospital. Under the leadership of Dr. Sherrill, the Crippled Children’s Hospital served the Birmingham community for over 20 years helping polio patients transition back into their daily lives. Once the disease was largely eradicated in late 1960’s the hospital became repurposed and in 1969 became part of the University of Alabama at Birmingham. The Crippled Children’s Foundation was later formed which continues its mission in fighting childhood diseases today. Though the original “Hospital Football Built” has since been torn down and UAB’s Spain-Wallace Building now stands in its place, the spirit of its presence remains. Since that time, over $29 million has been contributed by the club and the Crippled Children’s Foundation to charitable organizations.
Throughout its history, UAB orthopaedic surgery has had the benefit of strong leaders. Beginning with Dr. Sherrill, each leader of orthopaedic surgery, whether acting as Chief of Orthopaedic Surgery, Division Director of Orthopaedic Surgery, or ultimately Chairman of the Department of Orthopaedic Surgery, put their indelible mark on the growth and development of the orthopaedic program. The roster of the leaders of orthopaedic surgery is as follows:
Leaders of UAB Orthopaedic Surgery:
Chestley L. Yelton, MD 1963-1974
Kurt M. W. Niemann, MD 1974-1989
Victoria R. Masear, MD 1990-1994
John M. Cuckler, MD 1994-2004
Thomas R. Hunt, MD 2004-2012
Steven M. Theiss, MD 2013-present
The growth and development of orthopaedic surgery at UAB ultimately culminated in 2017 with it being elevated to Department status, becoming the 27th department at UAB. This designation not only recognized the maturation of the program, but also gave UAB Orthopaedic Surgery the resources needed to grow their clinical, education and research programs.
History of the UAB Department of Orthopaedic Surgery Residency
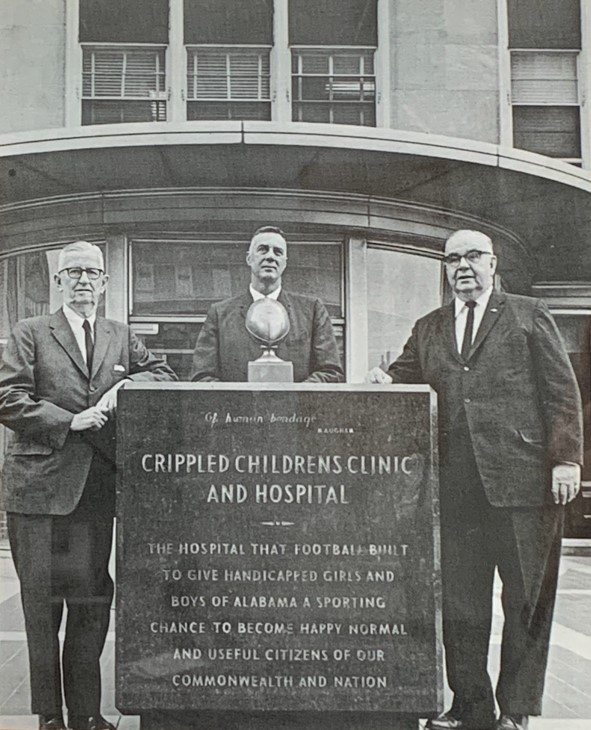 “The Hospital Football Built” monument. John D. Sherrill, MD (left). The orthopaedic surgery residency program started in the late 1940s. Ralph J.W. Hobbs, MD of Edenton, NC, was the first resident and later joined Dr. Sherrill in practice. There were several other notable residents during the early years of the program. These were notable not only for their distinguished careers in the Birmingham area, but also because of their historical family ties to orthopaedic surgery at UAB. These included Dr. Benjamin Meyer who was the second resident, and practiced most of his life at Carraway Methodist Hospital in Birmingham. Dr. John D. Sherrill, Jr., trained as a resident in the early 1950s, as the second member of the Sherrill family to be affiliated with UAB, joined his father’s practice and followed him as an orthopaedist for the University of Alabama football team. Finally, Dr. Joe Sherrill, Dr. John’s grandson, also finished the UAB orthopaedic residency in 1980 and practices orthopaedic and hand surgery in the Birmingham area. Dr. Richard Meyer, son of Dr. Benjamin Meyer, also finished his orthopaedic residency in 1976 and is on the orthopaedic surgery staff at UAB.
“The Hospital Football Built” monument. John D. Sherrill, MD (left). The orthopaedic surgery residency program started in the late 1940s. Ralph J.W. Hobbs, MD of Edenton, NC, was the first resident and later joined Dr. Sherrill in practice. There were several other notable residents during the early years of the program. These were notable not only for their distinguished careers in the Birmingham area, but also because of their historical family ties to orthopaedic surgery at UAB. These included Dr. Benjamin Meyer who was the second resident, and practiced most of his life at Carraway Methodist Hospital in Birmingham. Dr. John D. Sherrill, Jr., trained as a resident in the early 1950s, as the second member of the Sherrill family to be affiliated with UAB, joined his father’s practice and followed him as an orthopaedist for the University of Alabama football team. Finally, Dr. Joe Sherrill, Dr. John’s grandson, also finished the UAB orthopaedic residency in 1980 and practices orthopaedic and hand surgery in the Birmingham area. Dr. Richard Meyer, son of Dr. Benjamin Meyer, also finished his orthopaedic residency in 1976 and is on the orthopaedic surgery staff at UAB.
During the late 1960s and early 70s the orthopaedic residency program covered several hospitals including the University of Alabama at Birmingham, Birmingham Veteran Affairs Hospital, Children’s, the Cripple Children’s Service, Cooper Green, and Lloyd Nolan Hospital in Fairfield, AL. The orthopaedic residency at Lloyd Nolan Hospital in Birmingham was absorbed into the UAB program in 1971, which opened the UAB Orthopaedic Surgery residency to four residents each year in the four-year program. Ultimately, in 2004 under the leadership of Dr. Thomas Hunt, and Dr. David Volgas, the orthopaedic residency program increased the number of residents to six per year in the five-year program. This represents the current compliment of resident positions today. The present makeup of the program, including the service rotations, can be viewed here.
Five Orthopaedic Surgery faculty receive 2022 UAB Patient Experience Excellence Awards
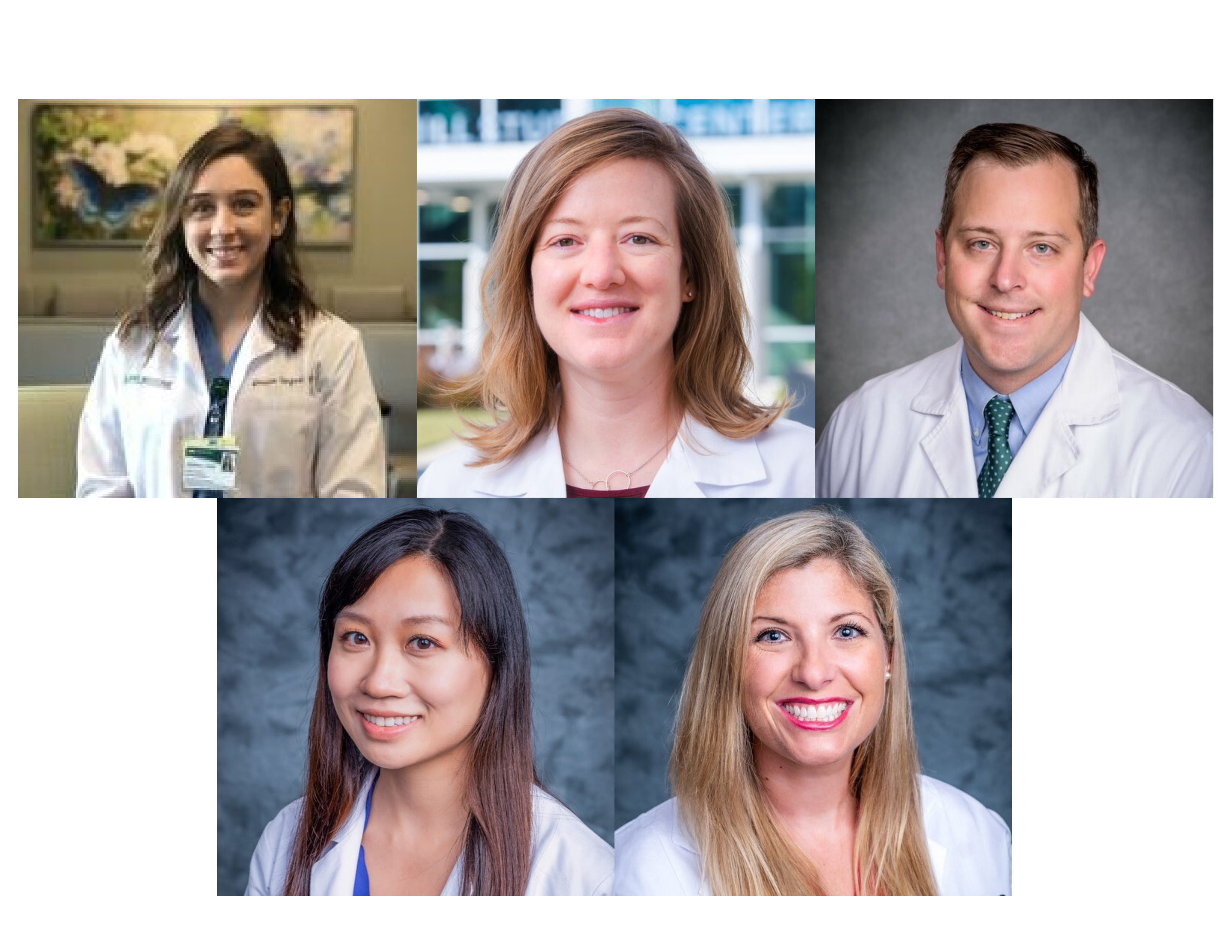
The UAB Medicine Office of Patient Experience and Engagement has awarded five Department of Orthopaedic Surgery faculty and staff 2022 Patient Experience Excellence Awards for their efforts in patient satisfaction.
The award recognizes UAB providers who received a 95% or higher in patient care, achieving top scores on the following metrics this past fiscal year:
• Listened carefully
• Demonstrated care and concern
• Provided clear explanations
• Included patient in healthcare decisions
• Overall care rating (0-10 scale)
Orthopaedic Surgery providers recognized include:
- Jessica S. Balik, CRNP
- Thomas B. Evely, DO, Assistant Professor
- Lisa Kafchinski, MD, Assistant Professor, Associate Program Director - Orthopaedic Surgery Residency Program
- Karlee Hiu Lau, MD, Assistant Professor
- Erin Ransom, MD, Assistant Professor