 Illustrations by Ernie Eldredge
Illustrations by Ernie Eldredge What do you want out of life?
For someone facing a serious, chronic illness, the answers to that question take on a sharp focus. A patient with heart disease might want enough energy to walk around the neighborhood. A cancer survivor may want to feel like herself again after rounds of chemotherapy. Others might have a goal of seeing their children get married—or perhaps to get married themselves.
Helping patients get the most out of life is the aim of palliative care—which could surprise some people who associate the specialty with hospice, or care delivered in the final days and hours. Palliative care services do indeed benefit people nearing the end of their journey, but the field has become much broader over time. Many patients with a life-threatening disease now start receiving palliative care early—sometimes soon after diagnosis—to support them throughout their fight. In fact, palliative care now ranks among the fastest growing medical specialties—67 percent of U.S. hospitals with 50 or more beds offer it, according to a 2015 report from the Center to Advance Palliative Care (CAPC)—in part because patients, families, and physicians like its emphasis on personalized treatment goals and quality of life.
Care + comfort
Perhaps the best way to understand the value of palliative care is to recall a time—not long ago—when such care was scarce. Marie Bakitas, D.N.Sc., remembers it well. Earlier in her career, before becoming the Marie L. O’Koren Endowed Chair and professor in the UAB School of Nursing and associate director of the UAB Center for Palliative and Supportive Care (CPSC), Bakitas wondered about the “invisible” patients—the ones who weren’t responding to pioneering cancer treatments. They didn’t have a lot of resources or support, she noted. Marie Bakitas and Rodney Tucker lead the UAB center providing an extra layer of support for patients dealing with serious illnesses.
Marie Bakitas and Rodney Tucker lead the UAB center providing an extra layer of support for patients dealing with serious illnesses.
Likewise, J. Nicholas Dionne-Odom, Ph.D., a School of Nursing postdoctoral fellow who worked as an intensive-care unit nurse for 10 years, saw patients and families navigating a traumatic “alien environment” of life-sustaining machines and uncomfortable procedures. “They often were dumbstruck,” he explains. “It was not how they imagined the end of their lives.”
The “extra layer of support” that palliative care provides can make all the difference, both physically and emotionally, Bakitas says. Teams of specialists focus on the patient’s comfort, managing symptoms such as pain, breathing issues, nausea, vomiting, and sleeping problems, to name a few examples, along with depression, anxiety, and spiritual issues. They also help patients and families make health-care decisions and plan for the future.
What these teams don’t do is replace a patient’s primary- or specialty-care physicians. Many patients concurrently receive treatments geared toward cure or remission, and the palliative care team works in tandem with their doctors. That’s the case with many cancer patients, says Rodney Tucker, M.D., director of the UAB CPSC. The same goes for “a heart-failure patient struggling earlier in the disease process, or a patient and family early in the diagnosis of Alzheimer’s disease who need a discussion about advance care planning and what to anticipate,” he adds. “Any patient with an illness that is life-threatening or life-limiting — one that causes severe decreases in quality of life — could benefit from palliative care.” Age, disease, and stage of disease progression do not matter.
“We’ve shown that people who engage in palliative care early and concurrently have improved survival rates,” Tucker says. “That’s the opposite of what many people think — that if I’m acknowledging my serious illness, then I’m giving up hope. When people are aware of all their choices, then they often select options that improve the quality of their lives when the quantity of their lives is limited.”
Symptoms, choices and goals
Here’s an example of one of those choices: Let’s say you’re a cancer patient with a normal life expectancy, but you’re dealing with the side effects from treatment. Is the best solution a medication with its own powerful side effects such as confusion or drowsiness? Or do you pursue other forms of symptom management with less impact on your day-to-day life?
 Specialist teams led by Ashley Nichols, left, and Elizabeth Kvale design palliative care plans to meet patient and family goals.
Specialist teams led by Ashley Nichols, left, and Elizabeth Kvale design palliative care plans to meet patient and family goals.
Elizabeth Kvale, M.D., might advise you to choose the latter. She directs the UAB Supportive Care and Survivorship Clinic, located at The Kirklin Clinic of UAB Hospital. UAB was among the first palliative care programs to establish an outpatient clinic, around 2000, and it’s where Kvale and her team help patients who are living with cancer, advanced heart disease, lung disease, or other serious conditions. Some of those patients still receive medical treatment for their chronic diseases, while others have completed it. Kvale and her colleagues help all of them manage symptoms. She compares the clinic to “a good corner man in a boxing match, who can keep patients patched up enough to stay in the fight if they want to do that.”
A few blocks away, another team, led by Ashley Nichols, M.D., staffs UAB Hospital’s 12-bed Palliative and Comfort Care Unit. Each room resembles a hotel suite, with comfortable leather couches, warm lighting, and wood accents—and the comparison is appropriate, Nichols says, because it is a “transitional unit.” Here, critically ill patients and their families have an option beyond the ICU while they are in the hospital, and for many of them, the next stop is their own home. “That’s where so many patients want to be,” says Nichols, a School of Medicine assistant professor. “So we work to control their symptoms, and we work with families and community hospice partners to develop a care plan to get them back home.”
Beyond the unit, Nichols and her group visit patients with every kind of disease throughout UAB Hospital, provide care at the Veterans Affairs Medical Center and Children’s of Alabama, and coordinate continued care with community hospice partners; they even do a few home visits. Typically, the team works with physicians on late-stage care, “but we’re also consulted more upstream—earlier in the disease process—when teams recognize an uncontrolled symptom burden, such as shortness of breath from chronic obstructive pulmonary disease, pain from a newly diagnosed cancer, or depression and anxiety associated with any chronic illness,” Nichols says. “If a symptom bothers patients, then it bothers us. We can partner with them and their physicians early and help manage symptoms throughout the course of the disease, as well as talk about goals for the patient’s care.”
Those goals are the key to quality palliative care, no matter the setting. What do patients want to accomplish—today, tomorrow, and in the rest of their lives? What kind of care will help them achieve their aims? Helping patients weigh the benefits of medical interventions against the potential costs to their quality of life, not to mention their pocketbook, is “the crux of what we do,” says Kvale, an associate professor in the School of Medicine. “Our objective is to align our care plan with patient and family goals. We also want to provide a space where it is OK for them to begin exploring other options, such as not seeking further invasive treatments.”
Strength in numbers
A hospital is not the easiest place to perform a full-immersion baptism, but UAB Pastoral Care chaplains have made it happen, thanks to an arrangement with UAB’s therapy pool. They also have officiated marriages for patients, complete with music and wedding cake; nurses helped one bride with a dress and makeup.
Mostly, though, they simply talk with patients about their sources of strength and the big questions that arise in tough times, sometimes without bringing up religion at all.
The chaplains are part of the interdisciplinary teams that staff the Palliative and Comfort Care Unit and the Supportive Care and Survivorship Clinic. Both groups bring together a variety of specialists who can help patients relax physically and cope mentally: physicians, nurses, psychologists, social workers, dieticians, physical therapists, music therapists, and even massage and pet therapists, in addition to spiritual care. In meetings, each professional provides a different perspective on what each patient needs; the result is a comprehensive, holistic, seamless care plan, Nichols says.
Teams also support families and caregivers. “Most of our patients live in the community and try to manage their illnesses with the help of a caregiver, so if we aren’t helping them engage with what’s going on with the patient, then the system is likely to fail,” Kvale says. “It’s a place where palliative care can have a big impact.”
A way forward
Listening may be the teams’ most powerful tool. When patients and families share their stories, they reveal much about their symptoms and quality of life—but also their joys, fears, loves, regrets, relationships, and unfinished business.
 Diane Tucker, left, and Kay Knowlton encourage patients and families to talk about grief, fear and the future.
Diane Tucker, left, and Kay Knowlton encourage patients and families to talk about grief, fear and the future.
“We listen with no agenda; we’re not trying to diagnose anything or resolve relationship issues,” says counselor Kay Knowlton, Ph.D. The overriding emotion is grief, she adds—grief over the end of life, or grief over life changes caused by illness. For example, a patient in the Supportive Care and Survivorship Clinic whose cancer is in remission might not look sick, but chemotherapy and radiation may have affected her sight, hearing, cognitive function, and ability to return to work.
“She’s coping with losses as well,” says Diane Tucker, Ph.D., a UAB psychology professor who also counsels palliative care patients. “She can’t go back to where she was before treatment.”
Diane Tucker and Knowlton help patients and families adjust to their new normal by talking with them about the future—how to move forward and accomplish what they consider important—without discounting the sadness, worry, or anger they might be experiencing. Tucker notes that suffering and pain are partly psychological. Helping patients handle their tension and fear can bring some relief.
Often, the psychologists help patients leave a legacy for their loved ones. Patients might write letters to their children or grandchildren, to be read when they are graduating from high school, getting married, or marking other milestones. Patients and families also can use the hospital unit’s art station to create a treasured memento.
Knowlton recalls helping one nine-year-old girl make handprints with her ill grandmother. The big and small handprints touched at the thumbs. “It didn’t mean that the girl wasn’t going to cry anymore, but it was a connection she needed because her grandma was leaving,” Knowlton says.
Likewise, the marriage ceremonies that the chaplains have performed create legacies for family members. Sometimes it means that the survivors can receive benefits. But these special moments also become pieces of family history that they can cherish for the rest of their lives.
Long-distance learning
Although palliative care has made great strides in recent years, millions more patients stand to benefit from it—if they can access it. The specialty is scarce or nonexistent in smaller hospitals, rural areas, and minority and underserved communities, says Bakitas. Alabama traditionally has ranked among the states with the lowest access, with less than one third of hospitals offering palliative care, according to the 2015 CAPC report. And there are a host of reasons why: lack of palliative care knowledge among health providers, socioeconomic factors, geographic distance, and transportation issues, among others.
Bakitas, along with Dionne-Odom, is bridging those gaps via telehealth—teaching palliative care principles to patients over the phone. Health coaches “show patients how to build upon the strengths of their personal, family, and community resources,” Bakitas says. They also talk about problem-solving and decision-making, self-care, early symptom management, communicating health concerns to clinicians, and emotional and spiritual topics. “We help people think about their illness in context,” she explains. “The illness is not who they are; it’s only a piece of their lives.”
Dionne-Odom develops telehealth programs for family caregivers as well as patients newly diagnosed with advanced illness. Caregivers often experience levels of stress and anxiety equal to—and sometimes greater than—those of patients, he notes. Talking with a health coach offers an outlet to express what they’re experiencing and to learn skills and coping abilities.
In fact, a recent study led by Dionne-Odom was the first to show that early palliative care benefits caregivers as well as patients. For caregivers of patients with advanced cancer living in rural areas, depression scores improved when those caregivers received palliative care via telehealth within a month after diagnosis, as opposed to those whose patients received care four months later. For patients in the study, one-year survival improved by 15 percent.
Now, with support from the National Palliative Care Research Center, Dionne-Odom is laying the groundwork for a new intervention to coach family caregivers at diagnosis, through the course of disease, and into bereavement. He hopes to implement the initiative in rural areas of Alabama and the Deep South.
Bakitas also is expanding her investigations with a $3.5-million National Institute of Nursing Research grant to study whether early palliative care, delivered by phone, can improve quality of life, mood, and symptom burden for advanced heart-failure patients and their caregivers. The American Cancer Society also awarded her a grant to study the impact of a phone-based intervention for veterans, minorities, and rural patients with advanced cancer.
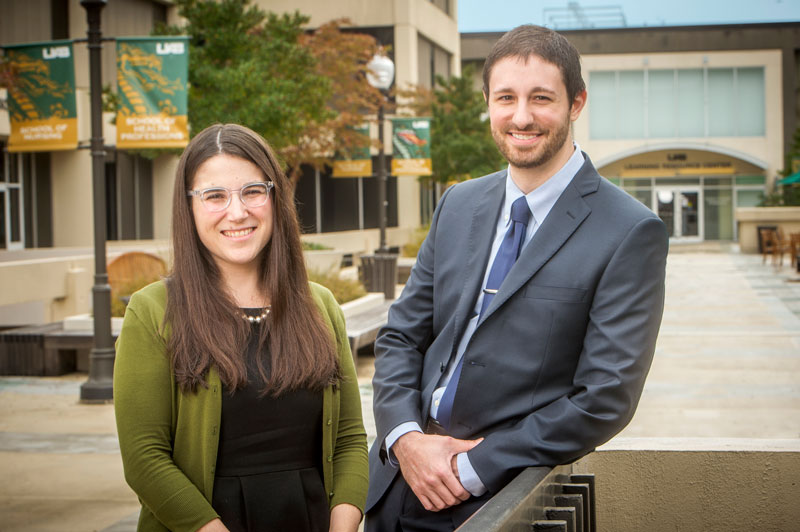 Jessica Merlin and J. Nicholas Dionne-Odom are adapting palliative care for rural areas and diseases such as HIV.
Jessica Merlin and J. Nicholas Dionne-Odom are adapting palliative care for rural areas and diseases such as HIV.
What patients want
UAB researchers also are expanding palliative care’s boundaries by adapting it for other serious diseases. Few specialists had studied the intricacies of chronic pain in patients with HIV before Jessica Merlin, M.D., M.B.A., began her work. “It’s not clear why there’s a lot of chronic pain with HIV,” says Merlin, assistant professor and director of the HIV Pain/Palliative Care Clinic at UAB’s 1917 Clinic. “Does something with HIV predispose patients to pain?” To complicate matters, some patients might experience chronic pain not caused by HIV, such as migraines or arthritis, and current medications aren’t entirely effective and may carry risks, she adds.
Now Merlin is developing an intervention—supported by a National Institutes of Health grant—that relies on behavioral therapy instead. “It’s unlikely that a pill can take away chronic pain, so we need to help patients put their pain in the background and themselves in the foreground,” Merlin explains. She envisions a program in which patients learn pain self-management skills from a trained provider.
“This is practical,” Merlin says. Medical research suggests that “when patients come to physicians and other providers, their highest priorities are treating pain and other symptoms.”
Lessons at the bedside
To ensure that health professionals understand quality-of-life issues, the UAB CPSC has a robust educational program. UAB students and residents in medicine, nursing, clinical psychology, and social work rotate through or intern in the clinic and hospital unit. For many, “this may be the first encounter with a patient who’s dying,” Nichols says. And that leads to important early lessons about discussing difficult end-of-life decisions with patients, handling anger and sadness from families, and responding personally to the loss of a patient. It also influences how future professionals look at life and death, Nichols adds. “Death is not a failure, but an opportunity to support patients and families.”
Physicians, nurses, and others seeking advanced training can join UAB’s specialized fellowship program or its clinical training academy, which has attracted professionals from as far away as Australia to observe UAB palliative experts at work. In addition, “we have trained 85 health-care institutions across the country and one in Korea about building business plans around palliative care,” Rodney Tucker says.
| "We've shown that people who engage in palliative care early and concurrently have improved survival rates" |
Reaching further
Palliative care will continue to grow and become more common throughout health care, say UAB’s experts. The field’s focus on patients and their goals offers a template for personalized medicine. And demand for it will rise as health care shifts toward “managing disease crises at home quickly and efficiently so that patients don’t need to come to the hospital,” Nichols says.
“We must learn better ways to partner with care organizations closer to the patient—including those that may not be considered palliative care, such as home-care organizations and skilled nursing facilities,” Rodney Tucker says. This year, the CPSC will establish the Southeast Institute for Innovation in Palliative and Supportive Care, which will educate health workers in communities throughout the region and conduct research to better understand the needs of seriously ill patients and families. Some of those initiatives may build on UAB’s pioneering work in telehealth and the training of lay navigators—people in community settings who can help patients make sense of the health-care system and their options.
While the new institute will give UAB a greater voice in the national conversation about palliative care, the specialists on UAB’s care teams feel privileged to help Alabama’s mothers and fathers, sons and daughters, and their families and friends maximize their lives when facing tough situations and choices.
“The truth is that none of us know how much time we have left,” Knowlton notes. “So what is today about? How can we live today in the best way possible?”
Pioneering a new kind of care
Some of the seeds for palliative care’s rapid growth were planted in the 1990s by a team led by UAB psychiatrist John Shuster, nurse scientist Pam Fordham, and medical oncologist Amos Bailey. Their partnership brought together the UAB schools of Medicine and Nursing and Cooper Green Hospital to promote clinical care, education, and research in the emerging field. The group soon established some of the nation’s earliest fellowship programs for physicians and training tracks for nurse practitioners.
Ten years ago, the UAB Center for Palliative and Supportive Care opened two clinical units, at UAB Hospital and the Birmingham Veterans Affairs Medical Center, within six months. At that time, when many major cities across the country barely had one inpatient palliative care facility, Birmingham had three, counting Cooper Green’s unit.
Nationally, UAB is one of only 11 Palliative Care Leadership Centers, which train and mentor other institutions launching their own clinical programs, and was among the first nursing education programs in palliative care. UAB also is a founding member of the national Palliative Care Research Cooperative Group.