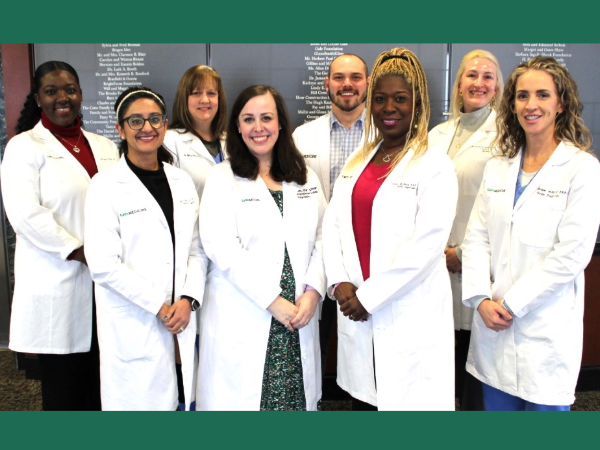
 Pictured: APPs in the UAB Department of Psychiatry and Behavioral Neurobiology, including Valisia Davis, DNP, CRNP, PMHS, PNP-BC, APP Supervisor; Leah Pickett, DNP, CRNP, APP Manager; Richard M. Hall, MSPAS, PA-C; Andrea "Cassidy" James Sharma, CRNP, FPMHNP-BC; Christine Fowler, MSN, PMHNP-BC; Amy Britton, FNP-C, ACNP; Sabah Angeles, MSN, PMHNP-BC; Aimee Morrison, Ph.D., PMHNP-BC; Not pictured: Bentley Adams, MSN, PMHNP-BC; Gwendolyn Allen, MSN, FNP-C; Jessica Skarda, MSN, PMHNP-BC; Donna Williams, MSN, PMHNP-BC.
Pictured: APPs in the UAB Department of Psychiatry and Behavioral Neurobiology, including Valisia Davis, DNP, CRNP, PMHS, PNP-BC, APP Supervisor; Leah Pickett, DNP, CRNP, APP Manager; Richard M. Hall, MSPAS, PA-C; Andrea "Cassidy" James Sharma, CRNP, FPMHNP-BC; Christine Fowler, MSN, PMHNP-BC; Amy Britton, FNP-C, ACNP; Sabah Angeles, MSN, PMHNP-BC; Aimee Morrison, Ph.D., PMHNP-BC; Not pictured: Bentley Adams, MSN, PMHNP-BC; Gwendolyn Allen, MSN, FNP-C; Jessica Skarda, MSN, PMHNP-BC; Donna Williams, MSN, PMHNP-BC.
In the UAB Department of Psychiatry and Behavioral Neurobiology, Advanced Practice Providers (APPs) are on the front lines of patient care, working in a capacity similar to physicians across a diverse range of clinical settings.
“APPs help to decrease the wait time for patients requiring an initial psychiatric evaluation in the clinic," said Valisia Davis, APP supervisor in the UAB Department of Psychiatry and Behavioral Neurobiology. "A plan of care is initiated for the management of current symptoms when seeing APPs because we have been empowered to function at the top of our license, which gives us the ability to independently care for patients seen in the clinic.”
Davis currently supports a team of a dozen APPs who work to provide personalized mental health care at UAB, focusing on advocacy, disease prevention, patient education, and empowerment. Richard Hall, MSPAS, PA-C, expanded on his role as a physician assistant on the team.
“We play a critical role in meeting the community’s overwhelming need for professional, competent, and uniquely compassionate mental health services,” Hall said. "I feel honored to be the first physician assistant (PA) in the department. PAs have not historically worked in the mental health field, beyond a scant few. I hope that my work here demonstrates the value of my profession and leads to further PAs joining the department in the future.”
Matthew Macaluso, D.O., Bee McWane Reid Professor and Vice Chair of Clinical Affairs, elaborates on APPs and their impact on patient care.
Q: What is an APP?
Macaluso: An Advanced Practice Provider (APP), typically a physician assistant or nurse practitioner, is a health care provider who is not a physician but performs many of the same duties as a physician, under a collaborative practice agreement with one or more physician supervisors. The Department of Psychiatry and Behavioral Neurobiology has expanded patient care access through hiring, advanced training, and collaboration with APPs.
APPs are generally physician assistants or nurse practitioners (NP). NPs earn master's or doctoral degrees in psychiatric-mental health nursing through graduate work. NPs may hold a doctoral degree, including either the Doctor of Nursing Practice or the Doctor of Philosophy degree. Physician assistants (PAs), on the other hand, are educated at the master’s degree level. PA programs are usually 27 months or three academic years in duration and include classroom instruction as well as hands-on clinical rotations.
Q: Why are APPs significant?
Macaluso: APPs work in all areas of health care and are critical to the patient care efforts at UAB Medicine and all around the United States. APP practice not only touches all medical specialties, but includes work in ambulatory as well as hospital settings, community mental health centers, emergency rooms, home health care, and residential settings. Behavioral health-focused APPs may specialize in the treatment of a particular population, such as geriatrics, child and adolescent patients, the seriously mentally ill (SMI), substance abuse disorders, or trauma-focused care, to name a few.
Q. What role do APPs play in the UAB Department of Psychiatry and Behavioral Neurobiology?
Macaluso: APPs in the Department of Psychiatry and Behavioral Neurobiology account for more than 1,000 arrived patient appointments each year plus important work on inpatient and hospital consultation services, as well as patient care at the Community Psychiatry Program and Beacon Recovery Program. We value and wish to grow our APP collaboration to continue the success of the same and promote continued expanded patient access.