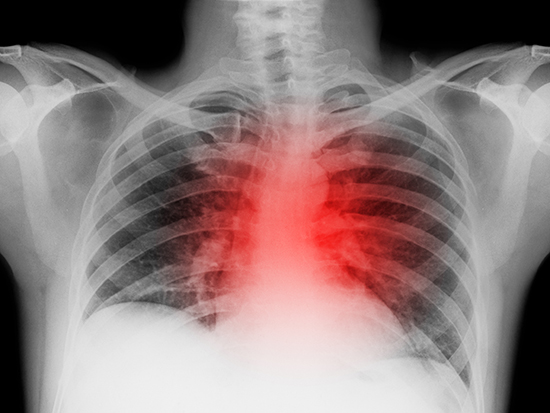
 Understanding how reductive stress is controlled may help personalize treatment of heart failure patients, leading to better outcomes.
Understanding how reductive stress is controlled may help personalize treatment of heart failure patients, leading to better outcomes.
Last year, University of Alabama at Birmingham researchers reported that reductive stress — an imbalance in the normal oxidation/reduction homeostasis — caused pathological changes associated with heart failure in a mouse model. This was a follow-up to their 2018 clinical study that about one in six heart failure patients shows reductive stress.
Now, in the journal Scientific Reports, researchers describe the putative molecular regulators of this pathological chronic reductive stress — a microRNA network.
Redox balance is vital for health. Oxidative stress has long been linked to heart failure, the progressive weakening of the heart muscle that can lead to death, though attempts at antioxidant therapy have been ineffectual. The finding that reductive stress can also lead to heart pathology may help personalize treatment of heart failure patients, leading to better outcomes.
Human microRNAs, or miRNAs, are short, non-coding RNAs with about 22 bases. They act to regulate gene expression by a complementary pairing with specific messenger RNAs of the cell. That pairing silences the messenger RNA, preventing them from being translated into a protein. Thus, miRNAs are a fine-tuned controller of cell metabolism or the cell’s response to stress and adverse challenges, like oxidative stress in the heart.
The current research, led by Rajasekaran Namakkal-Soorappan, Ph.D., associate professor in the UAB Department of Pathology, used mice that overexpress Nrf2, pronounced “nerf-two,” in cardiomyocytes to identify the miRNA network.
Nrf2 is a master transcriptional regulator that confers short-term protection — by helping express genes for antioxidant activity — for heart muscle cells when reactive oxygen and nitrogen species are created as blood flow returns after a heart attack. However, persistent Nrf2 activation can paradoxically result in reductive stress.
The researchers had recently shown that Nrf2 deficiency inhibited the expression of several miRNAs in the heart, suggesting a relationship between Nrf2 expression and miRNAs. So, they now decided to look for changes in miRNA levels in three mouse models — one with normal Nrf2 and two that constitutively overexpress Nrf2, at either low or high levels. Overexpression of both leads to pathological heart remodeling.
Comparison of miRNA levels from the three models identified a subset of miRNAs that appeared to be a direct and dose-dependent target of Nrf2, and thus putative regulators of reductive stress. Namakkal-Soorappan calls these miRNAs reductomiRs, pronounced “reducto-meers.”
The researchers also identified dose-dependent genes that were differentially expressed in the hearts of mice that overexpress Nrf2. Because miRNAs silence gene expression at the post-transcriptional level, the researchers believed that this distinct subset of genes could represent reductomiR targets for negative regulation.
Next, they looked for a link between the reductomiRs and the genes. In normal function, Nrf2 promotes the expression of genes that contain a DNA sequence called the “antioxidant response element” located near their promoters. With genomic software tools, the researchers probed the DNA of the mouse genome to find sequences for miRNAs that also had an antioxidant response element near their promoters.
 Rajasekaran Namakkal-Soorappan, Ph.D., associate professor in the UAB Department of Pathology.
Rajasekaran Namakkal-Soorappan, Ph.D., associate professor in the UAB Department of Pathology.
(Photography: Lexi Coon)They then used bioinformatics tools to identify 19 miRNAs that exhibited complementary sequences to the seed sequences in 61 down-regulated differentially expressed genes. These 19 miRNAs thus appear to be reductomiRs that mediate Nrf2-responsive myocardial reductive stress. Other computational tools also were used to create an integrative, Nrf2‑responsive miRNA-mRNA functional network that shows putative nodes of differentially expressed genes.
Namakkal-Soorappan calls the reductomiRs only putative mediators because the analyses in the current study resulted from bioinformatics. Needed next, he says, are mechanistic studies to confirm functions of the mediators.
Co-first authors of the study, “Identification of Nrf2‑responsive microRNA networks as putative mediators of myocardial reductive stress,” are Justin M. Quiles and Mark E. Pepin, UAB Department of Pathology, Division of Molecular and Cellular Pathology.
Co-authors, along with corresponding author Namakkal-Soorappan, are Sini Sunny, Sandeep B. Shelar, Anil K. Challa and Adam R. Wende, UAB Department of Pathology; Brian Dalley and John R. Hoidal, University of Utah; and Steven M. Pogwizd, UAB Department of Medicine Comprehensive Cardiovascular Center.
Support came from National Institutes of Health grants 2HL118067, HL118067, AG042860, HL133011, HL007918 and HL137240; American Heart Association grant BGIA 0865015F; a University of Utah Center for Aging Pilot Grant; the University of Utah; UAB; and an Alexander von Humboldt Foundation postdoctoral fellowship.